National Bowel Cancer Screening program
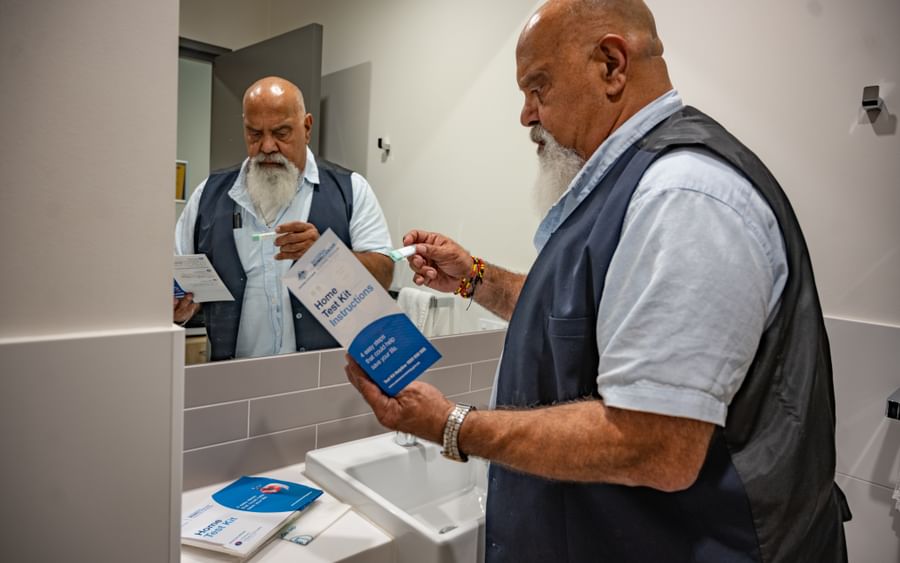
It’s recommended that all Australians aged 45 to 74 complete a bowel cancer screening test every two years as part of the National Bowel Cancer Screening Program.
The bowel cancer screening test is quick, clean and easy to do. It can find early signs of cancer, long before symptoms develop.
What is the bowel cancer screening test?
Bowel cancer screening involves completing an at-home bowel cancer screening test. The test looks for blood in your faeces (poo) that cannot be seen. If blood is found, you may need further testing to find the cause of the blood.
If you need help to complete your home test kit, call the Test Kit Helpline on 1800 930 998. You can also download instructions to complete your bowel cancer screening home test kit in other languages.
When should I do a bowel cancer screening test?
Australians aged 45 to 74 are eligible for the National Bowel Cancer Screening Program:
- People aged 50 to 74 will receive a free test kit in the mail every two years.
- As of 1 July 2024, people aged 45 to 49 can opt-in to receive their first free home test kit and join the National Bowel Cancer Screening Program by visiting ncsr.gov.au or calling 1800 627 701.
Bowel cancer screening tests are for people who do not have any symptoms. If you have symptoms that are unusual for you, see your doctor as soon as possible.
If you are not eligible for a free home test kit under the National Bowel Cancer Screening Program, speak with your doctor about other options suitable for you.
How do I get a bowel cancer screening test kit?
Visit the National Cancer Screening Register website or call 1800 627 701 to:
- request your first free home test kit be mailed to you, if you are 45-49 years old
- order a replacement test if you have lost or damaged your home test kit, or if it has expired.
For more information about cancer screening tests, call Cancer Council 13 11 20 to speak with an experienced cancer nurse.
What bowel cancer symptoms should I look for?
No matter your age, it’s important to know your body and what is normal for you. If you notice any of the following symptoms and they are unusual for you, you should see your doctor:
- Blood in your faeces (poo) or on the toilet paper.
- Unexplained changes in bowel habits such as diarrhoea, constipation or smaller, more frequent bowel movements.
- A change in the look of faeces (e.g. narrower or with mucus).
- Feeling fullness or bloating in the abdomen or a strange sensation in the rectum, often during a bowel movement.
- Feeling that the bowel hasn’t emptied completely after you have done a poo.
- Losing weight without trying.
- Weakness or fatigue.
- Rectal or anal pain.
- A lump in the rectum or anus.
- Abdominal pain or swelling.
- A low red blood cell count (anaemia).
- A blockage in the bowel, which is rare.
Not everyone with these symptoms has bowel cancer, and they may be due to other health conditions. Changes in bowel function are common and do not always indicate a serious problem. However, any amount of bleeding is not normal, and you should see your doctor for a check-up.
Who is at risk of developing bowel cancer?
Research shows that people with certain risk factors are more likely to develop bowel cancer. If you think you are at an increased risk of bowel cancer or have any concerns, see your doctor.
Risk factors for bowel cancer include:
- older age – most people with bowel cancer are over 50, and the risk increases with age
- polyps – having many polyps in the bowel
- bowel diseases – people who have an inflammatory bowel disease, such as Crohn’s disease or ulcerative colitis, have a significantly increased risk, particularly if they have had it for more than eight years
- lifestyle factors – being overweight, having a high intake of red meat or processed meats such as salami or ham, having a low dietary fibre intake, drinking alcohol, being sedentary and smoking are all linked with an increased risk of bowel cancer
- strong family history – a small number of bowel cancers run in families
- other diseases – people who have had bowel cancer once are more likely to develop a second bowel cancer; some people who have had ovarian or endometrial (uterine) cancer may have an increased risk of bowel cancer
- rare genetic disorders – a small number of bowel cancers are associated with inherited genes.
Family history of bowel cancer
If one or more of your immediate family members (such as a parent, sibling or child) have been diagnosed with bowel cancer, this may increase your risk of bowel cancer. This is especially the case if they were diagnosed before the age of 55, or if there are two or more close relatives on the same side of your family with bowel cancer.
A family history of other cancers, such as endometrial (uterine) cancer, may also increase your risk of developing bowel cancer.
There are two very rare genetic disorders that can run in families and are associated with an increased risk of bowel cancer. About five to six per cent of bowel cancers are caused by these inherited genetic conditions:
- Familial adenomatous polyposis (FAP) – This condition causes many polyps to form in the bowel. If left untreated, those with FAP are extremely likely to be diagnosed with bowel cancer in their lifetime (usually by the age of 40).
- Lynch syndrome – This syndrome is characterised by a fault in the gene that helps the cell’s DNA repair itself. It may increase the risk of bowel cancer or other cancers.
If you are concerned about bowel cancer because of your family history, see your doctor to discuss the need for regular check-ups or whether genetic testing would be suitable for you.
How can I reduce my risk of bowel cancer?
Research suggests that many cases of bowel cancer could be prevented by leading a healthy lifestyle. Your most effective protection against bowel cancer is to:
- complete a bowel cancer screening test every two years from age 45
- get 30 minutes of vigorous or 60 minutes of moderate intensity exercise on five or more days per week
- maintain a healthy body weight
- eat a fibre-rich, well-balanced diet
- avoid processed meat
- choose small amounts of lean red meat, or swap for chicken, fish or vegetarian options
- avoid or limit alcohol
- quit smoking.
For more information about how you can reduce your risk of bowel cancer, see your doctor or call Cancer Council SA on 13 11 20.