Cancer and the heart
Advances in cancer diagnosis and treatment mean more people are living longer after cancer treatment. This is good news, but research shows that cancer survivors have a higher risk of cardiovascular disease in the months and years after cancer treatment.
Cardiovascular disease includes problems with the heart and blood vessels. It may also be called heart disease.
There are several reasons why heart health is an important part of cancer treatment:
- Cardiovascular disease has the same risk factors as some types of cancer, so you may have a higher risk of developing both diseases.
- If you had cardiovascular problems before cancer (pre-existing disease), some cancer treatments may not be safe or may need to be used at a reduced dose.
- Some cancer treatments can affect the way the cardiovascular system works. This is called cardiotoxicity or cardiovascular toxicity.
- Some cancers (e.g. blood cancers, lung cancers) can increase the risk of blood clots and bleeding.
Heart-related side effects from cancer treatments are common, but serious issues are uncommon. The type of side effect and how common it is, depends on the cancer, its treatment and if you already have cardiovascular disease. These side effects usually go away after treatment, but some can be permanent. It’s important to tell your treatment team about any symptoms as soon as possible.
For most people, cancer treatment can save lives, and the benefits are greater than the risk of heart-related side effects. There are many ways to reduce your risk of heart problems.
The heart and cardiovascular system
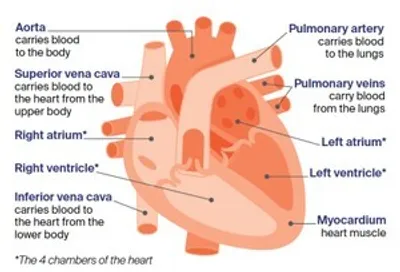
The heart is about the size of a fist. It is made up of muscle, blood vessels, nerves and valves. The heart is the main organ of the cardiovascular system, which also includes a network of blood vessels (arteries and veins) throughout the body. The heart has 4 chambers: the right atrium, the right ventricle, the left atrium and the left ventricle.
The heart pumps blood through the blood vessels to deliver oxygen and nutrients to cells in the body, and take away waste. Electrical signals tell the heart when to beat.
Key questions
Answers to some key questions about heart health and cancer are below.
What are the shared risk factors for cancer and heart disease?
Cancer and heart disease have some of the same risk factors. These shared risk factors include:
- older age
- your sex
- smoking
- diabetes
- physical inactivity
- drinking too much alcohol
- unhealthy diet
- high blood pressure (called hypertension)
- overweight and obesity
- high cholesterol (a type of fat in the blood)
- other chronic inflammatory conditions (e.g. chronic kidney disease).
Making some changes in your day-to-day life can help to lower the risk of heart-related side effects from cancer treatment. Some changes can also reduce the risk of certain cancers. Visit our prevention pages for tips about lifestyle changes. Heart Foundation also has information about looking after your heart.
What cancer treatments may affect the heart?
Some types of cancer treatment can affect how the heart and cardiovascular system work. This is called cardiotoxicity or cardiovascular toxicity.
When working out the best treatment for you, your doctors will try to find a therapy that is effective in treating the cancer while causing the least amount of damage to the heart and blood vessels. You may also be advised to do more physical activity and eat a healthy diet.
Cancer treatments that may be cardiotoxic include:
- certain chemotherapy drugs, particularly anthracyclines (e.g. doxorubicin, daunorubicin,
epirubicin) and thymidylate synthase inhibitors (e.g. fluorouracil or 5-FU) - some targeted therapy drugs (e.g. trastuzumab, bevacizumab, ribociclib, cabozantinib)
- some immunotherapy drugs (e.g. pembrolizumab, nivolumab, CAR T-cell therapy)
- radiation therapy to the chest for some types of cancer (e.g. breast, lung cancers or lymphoma).
These treatments can affect cardiovascular health in different ways.
Some treatments don’t directly affect the heart but can still impact cardiovascular health. For example, certain hormone therapies, such as aromatase inhibitors and androgen deprivation therapy, can increase the risk of high blood pressure, high cholesterol and high blood sugars.
What if you already have heart disease?
As cancer and heart disease often share risk factors, some people already have heart problems when they are diagnosed with cancer. In these cases, cancer treatments that are potentially cardiotoxic may not be safe. Your doctor may suggest other treatments.
If you’re taking heart medicine, it’s important to keep taking it until you discuss this with your cancer treatment team, cardiologist or cardio-oncologist. Also, let your cancer treatment team know if you have a pacemaker, so they can consider this when planning treatment.
"I had heart issues before being diagnosed with cancer (first primary breast cancer then, 9 years later, primary uterine sarcoma). Before starting chemotherapy for uterine sarcoma, my cardiologist and medical oncologist had a big discussion. They decided the planned chemo protocol would be okay.” Cynthia
What are some common heart problems linked to cancer and its treatment?
Angina and heart attack
What it means – When fats or other substances build up in the blood, blood vessels can become blocked (atherosclerosis). This can reduce the amount of blood flowing through the heart. It may cause:
- angina – pain or tightness in the chest when not enough blood is flowing to the heart. This needs to be checked because it may also be a symptom of a heart attack
- heart attack – pain in the chest due to permanent damage to the heart. This needs emergency treatment.
Risk may increase with some types of:
- chemotherapy
- immunotherapy
- radiation therapy to the chest for certain cancers
Blood clots
What it means – Blood clots are clumps of blood that can block blood vessels. They may cause serious conditions including:
- stroke – when the blocked blood vessel restricts blood flow to the brain (called an ischaemic stroke). Strokes can also be caused by bleeding in the brain if an artery leaks or splits (called a haemorrhagic stroke)
- pulmonary embolism (PE) – when a blood clot blocks the supply of blood to the lungs; this can be life-threatening
- deep vein thrombosis (DVT) – when a blood clot forms in a deep vein, often in the leg; can lead to pulmonary embolism.
Risk may increase with some types of:
- cancer
- chemotherapy
- hormone therapy
- immunotherapy
- ports, etc.
- radiation therapy to the chest for certain cancers (may increase stroke risk, not PE or DVT)
- surgery
- targeted therapy
Heart failure
What it means – Damage or weakening of the heart muscle (cardiomyopathy) may mean the heart becomes too weak to pump blood around the body properly. This can cause shortness of breath and fatigue. Cardiomyopathy must be treated quickly to prevent it becoming permanent.
Risk may increase with some types of:
- chemotherapy
- immunotherapy
- radiation therapy to the chest for certain cancers
- targeted therapy
Heart inflammation (myocarditis)
What it means – When the heart muscle (myocardium) becomes inflamed (swollen or irritated) it can affect the heart’s ability to pump blood. This may cause chest pain, shortness of breath and rapid or irregular heartbeats, and can be life-threatening if not treated early.
Risk may increase with some types of:
- immunotherapy
- radiation therapy to the chest for certain cancers
Irregular heartbeats (arrhythmia)
What it means – The heart has an electrical system that tells it to beat. If this system is not working properly, it can lead to a heartbeat that is irregular (beating too fast or too slow). This is called arrhythmia. For example, atrial fibrillation (AF) is an irregular heartbeat that is often faster than usual. Arrhythmia can cause you to be light-headed or dizzy and, in some cases, to faint. It may also be a sign of heart attack, heart failure or heart inflammation (myocarditis).
Risk may increase with some types of:
- chemotherapy
- immunotherapy
- radiation therapy to the chest for certain cancers
- targeted therapy
Other cardiovascular concerns
What it means – Cancer treatments may also affect the heart by causing:
- high blood pressure (hypertension) – when the force of the blood pushing against the artery walls is too high for a long time or the arteries become stiff, the heart has to work harder to pump blood. This increases the risk of heart attack and stroke
- high cholesterol (hyperlipidaemia) – a build-up of fats (lipids) in the blood. This increases the risk of heart attack, stroke and kidney damage
- high blood sugars (hyperglycaemia) – when there is too much glucose (sugar) in your blood. This increases the risk of heart attack, angina and stroke.
See your GP for regular check-ups for these issues.
Risk may increase with some types of:
- chemotherapy
- hormone therapy (e.g. androgen deprivation therapy)
- immunotherapy
- targeted therapy
What are the symptoms to look out for?
Watch for early signs that something may be wrong with your cardiovascular system. Some symptoms may not be related to the cancer or its treatment; your doctor will consider other possible causes.
Chest pain or tightness – This may feel like heavy, crushing pain or pressure in your chest, back, neck or jaw. It may also feel like sharp, stabbing pain.
Shortness of breath – This is when you feel that you cannot get enough air into your lungs. It’s normal to feel this way after exercise or physical work, but if it feels worse than usual or happens for no reason, this may be a sign of heart problems.
Swelling in the legs – If your heart is not pumping blood around the body as well as it should, blood and other fluids can build up in your legs, ankles and feet. This is called oedema. It can also be a side effect of some cancer treatments.
Fatigue – This is extreme tiredness and lack of energy that usually does not go away with rest.
Feeling faint or dizzy – You may feel light-headed, unsteady on your feet, or notice changes in your vision.
Abnormal heartbeat – Your heart may beat faster than usual (heart palpitations) or in an abnormal way (irregular heartbeat). This may happen when the heart’s electrical signals aren’t working properly.
Other symptoms – These may include: pain in the arms or shoulders; indigestion; unexplained
perspiration (feeling sweaty); or unexplained nausea (feeling sick) and vomiting. These symptoms are more common in women, but can also affect men. For more information about heart health for women, visit Her Heart.
If symptoms are severe or come on suddenly, call Triple Zero (000) or go to your nearest emergency department. Be sure to tell the emergency doctors about your cancer treatment.
Who are the health professionals I may see?
Looking after your cardiovascular health during and after cancer treatment is important. If you have existing heart problems or have any risk factors, you may need support in making lifestyle changes. You may see a:
- general practitioner (GP) – a doctor who supports your general health, including your cardiovascular health, before and after cancer treatment. Depending on where you are having your treatment, your GP may also be involved in your care during cancer treatment. If you don’t have a regular GP, it’s a good idea to find one and start building a relationship
- exercise physiologist, physiotherapist – prescribe safe and effective exercise to help restore or improve people’s overall health, fitness, strength and energy levels
- dietitian – helps with nutrition concerns and may recommend changes to your diet during treatment and recovery.
If you have a higher risk of heart-related side effects, you may also see a:
- cardiologist – a doctor who specialises in the treatment of heart disease
- cardio-oncologist – a cardiologist with special training in managing the effects of cancer and cancer treatments on the cardiovascular system; they help to reduce cardiovascular risks and manage cardiovascular problems that may occur
- cardiac nurse – a nurse who specialises in cardiovascular health; may be involved in some heart tests.
After your cancer treatment is finished, your heart health may continue to be monitored by your GP, a cardiologist or cardio-oncologist.
There are also many things that you can do to look after your own cardiovascular health and reduce your risk of any future problems.
What are some of the ways to keep your heart healthy?
Changing some daily habits can help to improve your heart health.
Starting healthier habits before cancer treatment (prehabilitation) and continuing them during and after treatment (rehabilitation), may help your recovery. Some changes can also help to prevent the cancer coming back. If your general practitioner (GP) refers you to see an allied health professional (e.g. exercise physiologist, dietitian), you may be eligible for Medicare rebates for some visits.
Sit less and be physically active
Spending too much time sitting can increase your risk of heart problems. Including regular movement and exercise in your daily or weekly routine is one of the most important changes you can make to lower your heart disease risk. It can also reduce cancer risk. It’s recommended that people with cancer work towards, then maintain, at least 150 minutes (2½ hours) of moderate-intensity aerobic exercise or 75 minutes (1¼ hours) of vigorous-intensity aerobic exercise every week. Aerobic exercise includes activities such as brisk walking or bike riding. Also, doing 2–3 strength-training (resistance exercise) sessions a week can build muscle strength. Even small increases in your activity levels can be good for your health.
Download our booklet ‘Exercise for People Living with Cancer’
Quit smoking and vaping
If you smoke or vape, it’s important to quit. Exposure to tobacco smoke can cause your blood vessels to become stiff and more likely to split. This can lead to angina, heart attack or stroke. Smoking also increases the risk of developing many types of cancer. It’s also important to avoid second-hand smoke and to stop vaping (e-cigarettes), which can harm your heart as well. For support, visit Quit, call the Quitline on 13 7848 or talk to your GP.
Maintain a healthy body weight
Carrying extra body weight can cause fatty material to build up in your blood vessels (atherosclerosis). This increases the risk of heart problems and stroke. While some people lose weight during cancer treatment, others gain weight due to side effects of some medicines. Talk to your cancer treatment team or GP about healthy eating and staying active to help manage your weight.
Drink less alcohol
Alcohol does not protect the heart, and drinking alcohol increases the risk of cancer. It’s important not to drink too much alcohol both for your heart health and to reduce the risk of some cancers (including breast, bowel, liver, mouth and stomach cancers). If you choose to drink, follow the Australian Government’s alcohol guidelines and limit alcohol use. If you do not drink alcohol, you should not start.
Eat a healthy diet
Eat a balanced diet from the 5 food groups – vegetables, fruit and legumes, breads and cereals, meat (and alternatives) and dairy (and alternatives). Limit foods containing saturated fat, added salt and added sugars, and avoid sugary drinks. Your doctor may suggest you see a dietitian to help you with your diet.
Download our booklet ‘Nutrition for People Living with Cancer’
Take your medicine
If you take heart medicines (for blood pressure or cholesterol) or diabetes medicines, keep taking them during and after cancer treatment, unless your doctors tell you to stop. If you have questions, talk to your doctor.
See your GP for heart checks
It’s important to get your blood pressure, blood sugar and cholesterol checked regularly,
including before, during and after cancer treatment. Talk to your GP about these tests.
Prevention and monitoring
Before treatment
Your heart health may be checked before you start cancer treatment. It’s important that your treatment team knows about any existing heart problems or risk factors (e.g. high blood pressure, high cholesterol, diabetes) so they can recommend the safest and most effective cancer treatment for you.
The doctor may ask you about your risk factors for developing heart problems and any previous heart issues or cancers you’ve had. They may also suggest changes you can make to improve your heart health.
To work out your overall risk of heart problems, your doctors will consider:
- your heart health before treatment
- any risk factors you have
- if the cancer treatments could affect your heart.
If you don’t have heart concerns and your treatment plan does not include treatments that might affect your heart, you may not need to have any heart tests.
If you have risk factors for cardiovascular disease or are receiving cancer treatment that may affect your cardiovascular system, then you may need some tests. You may have these before cancer treatment starts (called baseline tests). Any further tests can then be compared with the results of baseline tests to check for any changes in your heart during and after treatment.
Cardiovascular tests you may have before treatment
Depending on the type of cancer you have and your cardiovascular risk factors, you may have one or more of the following tests before starting cancer treatment.
Blood tests
What does it check for? If your heart has existing damage or is under strain, the cells may release particular proteins (called biomarkers) into the blood.
How it is done – A sample of your blood will be collected with a needle from a vein in your arm. It will be sent to a laboratory where a pathologist will check your blood for certain biomarkers.
Electrocardiogram (ECG)
What does it check for? This shows how fast or slow your heart is beating and checks for irregular heartbeats (called arrhythmias). It can also show if you have had a heart attack.
How it is done – Several leads (electrodes) will be stuck to your chest; any hair on your chest may need to be shaved so the electrodes stick properly. The electrodes are connected to a computer that records your heart beating.
Echocardiogram (echo scan)
What does it check for? This looks at how well your heart muscle and heart valves are working.
How it is done – This is a type of ultrasound scan. The person doing the ultrasound (sonographer) will spread gel on your chest and then move a small device (transducer) over the chest. The transducer sends soundwaves to a computer to create pictures of your heart.
Cardiac magnetic resonance imaging (CMRI)
What does it check for? This scan may be done if an echo scan suggests a more serious cardiovascular problem. A CMRI shows how well the heart is pumping and if the valves are working properly. Most people will not need this test.
How it is done – This scan uses a powerful magnet and radio waves to create detailed cross-sectional pictures of your heart. During the scan, you may be injected with a dye (called contrast) to help make the pictures clearer. You will lie on a table inside a large metal tube that is open at both ends. The scan is noisy but painless.
Computerised tomography (CT) coronary angiogram
What does it check for? This scan checks for any blockages or damage in your heart and surrounding blood vessels. It may be called a CTCA.
How it is done – A small tube (cannula) will be put into a vein in your arm. You will lie on a table that slides into the CT machine. Dye (called contrast) will be injected into the cannula to help show if there is any narrowing or blockage in your heart arteries. You will be asked to hold your breath for about 10 seconds and stay still while the images are taken.
Coronary angiogram
What does it check for? This test is used to check if the arteries around your heart (coronary arteries) have narrowed or are blocked. Most people will not need this test.
How it is done – A thin, flexible tube (catheter) is inserted into the largest artery in your body (the aorta) through your wrist or the groin. It is then threaded up into the coronary arteries. A dye (called contrast) is injected into the catheter, and x-rays are taken to show up any blockages.
Exercise stress test
What does it check for? This measures how well your heart and lungs are working during exercise.
How it is done – Your heart rhythm and lung function will be monitored while you walk on a treadmill or ride a stationary bike. The appointment may take about 90 minutes, but you will only be exercising for 5–15 minutes. An echo scan might be done before and after the stress test. You will be given instructions on what you can eat or drink the day before the test.
During and after cancer treatment
After having some of the tests listed above, your risk of developing heart problems will be assessed as low, moderate, or high and very high. This helps your doctors work out a treatment plan, and how closely to monitor your heart during and after your treatment.
Your heart risk may change over time. It’s important to tell your GP or cancer treatment team if you notice any symptoms that could be related to your heart. When found early, heart problems can usually be managed and are less likely to become serious.
Ways heart problems are managed
When planning the cancer treatment, your doctor will consider your risk for heart problems, the type of cancer treatment you need and the results from any heart tests.
If there are concerns about your heart health, your doctor may:
- change the type of cancer treatment to reduce the impact on the heart
- reduce the dose of the cardiotoxic drug so it works well against the cancer but is less likely to cause heart damage
- change how the drug is given. For example, chemotherapy given through a vein in your arm (intravenously) may be delivered more slowly
- prescribe heart medicines to be taken during, and sometimes after, cancer treatment. These can be to treat existing heart problems or to prevent them from developing. Research in this area is ongoing and new drugs may become available. Your doctor will talk to you about the best heart medicine for you.
Heart protection during radiation therapy
Radiation therapy has improved over time. Lower doses of radiation are now used to effectively treat the cancer while reducing the risk to other organs, including the heart.
If you need radiation therapy to the chest (e.g. for breast or lung cancer), the heart can be protected. Shielding in the radiation machine (called a linear accelerator) may be used to block radiation reaching the heart.
A special breathing technique is sometimes suggested. This is called a deep inspiration breath hold (DIBH). You will be asked to take a deep breath and hold it for about 20 seconds while the radiation is given. This technique helps move your heart away from the treatment area, protecting it from the radiation beams.
Even if many years have passed since the cancer treatment, always tell your health professional that you have had cancer and any treatments you had. Cancer will always be part of your medical history.
Question checklist
It’s important to understand the best ways to look after your heart health during cancer treatment.
Asking questions can help. You may want to include some of the questions below in your own list.
Before treatment
- Do I need cardiovascular tests before starting cancer treatment?
- What can I do to improve my heart health?
- What tests and scans do you recommend?
- When is the best time to have these tests?
- Is the cancer drug therapy recommended for me likely to affect my heart? Are there other treatments that are just as effective for the cancer but less likely to affect my heart?
- Is the radiation therapy recommended for me likely to affect my heart? What can be done to reduce the risk of heart damage?
During and after treatment
- Will my heart be monitored during and after cancer treatment?
- What tests will I have and how often will I have them?
- Will I have a follow-up plan and will it be shared with my GP?
- Who should I contact if I develop any symptoms that may be related to my heart?
- How will I know if I need to go to the emergency department or call Triple Zero (000)?
- If I develop heart problems, how will they be treated? What can I do to reduce the risk of heart problems after cancer treatment?
Featured resource
This information was last reviewed June 2025 by the following panel
Prof Bogda Koczwara, Director, Australian Research Centre for Cancer Survivorship, UNSW, NSW; Prof Aaron Sverdlov, Cardiologist and Co-Director, Newcastle Centre of Excellence in Cardio-Oncology, Hunter New England Health and The University of Newcastle, NSW; Dr Diana Adams, Medical Oncologist, Macarthur Cancer Therapy Centre, NSW; Tamara Casey, Clinical Nurse Consultant, Breast Assessment Unit, Fiona Stanley Hospital, WA; Dr Daniel Chen, Cardiologist and Specialist in Cardio-Oncology, Prince of Wales and St George Hospitals, NSW; A/Prof Eng-Siew Koh, Radiation Oncologist, Liverpool Cancer Therapy Centre, Liverpool Hospital and University of NSW, NSW; Cynthia Leigh, Consumer; Dr David Mizrahi, Senior Research Fellow and Accredited Exercise Physiologist, The Daffodil Centre at Cancer Council NSW and The University of Sydney, NSW; Prof Doan Ngo, Co-Director, Newcastle Centre of Excellence in Cardio-Oncology, The University of Newcastle, Hunter Medical Research Institute, NSW; Peter O’Hearn, Consumer; Prof Nick Pavlakis, Medical Oncologist, Royal North Shore Hospital and Professor of Medicine, The University of Sydney, NSW; Deb Roffe, 13 11 20 Consultant, Cancer Council SA; Dr Lorcan Ruane, Cardiologist, The Prince Charles Hospital, QLD; Margaret Ryan, Nurse Practitioner, Cardio-Oncology Clinic, Prince of Wales Hospital, NSW; Dr Elysia Thornton-Benko, Specialist GP/Primary Care and Cancer Survivorship Physician, NSW; Helen Wardman, Consumer; Dr Trent Williams, Clinical Nurse Consultant, Cardiology, John Hunter Hospital, NSW; Dr Janice Yeh, Radiation Oncologist, Peter MacCallum Cancer Centre, VIC; Megan Yong, Consumer.