National Cervical Cancer Screening Program
Regular cervical screening tests give you the best chance of detecting cancer early and ultimately, saving your life. A screening test can detect changes in your body long before cancer develops and treatment for these changes is very effective in preventing most cases of cervical cancer.
A cervical screening test is recommended every five years if you are:
- a woman or someone with a cervix
- aged 25 to 74
- someone who has ever been sexually active.
What is a cervical cancer screening test?
A cervical screening test involves taking a swab of the cervix or vagina to look for the presence of HPV, which causes 90 per cent of cervical cancers.
Most cases of HPV clear up on their own and do not require treatment. However, if some types of HPV remain in the body for a long time, they can cause changes to your cells including cervical cancer. If the cervical cancer screening test does find HPV, treatments are very effective at preventing cervical cancer.
The cervical screening test swab can be done by a doctor or nurse, or you can now choose to collect your own sample (known as self-collection) using a special type of long handled cotton bud, in private.
What is self-collection for cervical screening?
Anyone who is eligible for a cervical screening test can now choose between self-collection or having a sample collected by a doctor or nurse:
- A self-collection test uses a long-handled cotton bud to collect your own sample from the vagina. You can take this test in private at the doctor’s clinic or in some circumstances, at home.
- A sample collected by a doctor or nurse involves inserting a speculum to collect cells from the cervix.
The self-collection test is easy to do and just as safe and effective as having the test done by a doctor or nurse.
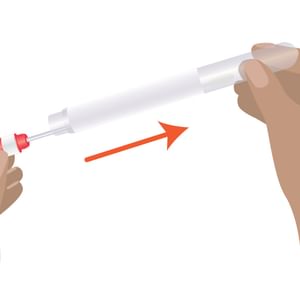
Here are four simple steps to do the self-collection for cervical screening test:

Step 1:
Twist the red cap and pull out the swap. Look at the swab and note the red mark closest to the tip.

Step 2:
Get in a comfortable position. Insert the swab into your vagina, aiming to insert to the red mark.

Step 3:
Rotate the swab gently one to three times.
Step 4:
Remove the swab and place back in the tube. Return it to your doctor, nurse or Aboriginal Health Worker. Contact the clinic for your results in two weeks.
Where can I have a cervical screening test?
You can have a cervical screening test at:
- a doctor’s clinic
- some women’s health centres and community health centres
- home, via SHINE SA’s telehealth service (eligibility criteria applies).
If it has been five or more years since your last cervical screening test, make sure to book an appointment with your doctor or women’s health clinic. If you would prefer to do a self-collected test, ask if self-collection is available at your clinic.
What cervical cancer symptoms should I look for?
Even if you are up to date with your cervical screening tests, it’s still important to see your doctor if you are experiencing symptoms that are unusual for you. These symptoms could be something other than cervical cancer, but it’s best to rule it out.
Cervical cancer symptoms may include:
- vaginal bleeding between periods, after menopause, or during or after sex
- pelvic pain
- pain during sex
- a change to your usual vaginal discharge (e.g. there may be more discharge than usual, or it may have a strong or unusual smell or colour).
Who is at risk of developing cervical cancer?
Almost all cases of cervical cancer are caused by HPV, which is very common virus. About four out of five people will be infected with at least one type of genital HPV at some point in their lifetime. Most people won’t know they have HPV because it doesn’t cause symptoms – that’s why cervical screening is so important.
Vaccination can prevent HPV and is available to all children aged 12-13 years for free as part of the National Immunisation Program. If you missed out on the HPV vaccination offered at school, you can catch up on the vaccination for free before you turn 26. The vaccination is recommended before you become sexually active.
Anyone with a cervix aged 25 to 74 should still have a cervical screening test every five years – even if they have had the HPV vaccine.
Other risk factors that may increase the risk of developing cervical cancer
- Smoking and passive smoking - Chemicals in tobacco can damage the cells of the cervix, making it harder for the body to clear the HPV infection.
- Using the oral contraceptive pill for a long time - Research has shown that taking the pill for five years or more increases the risk of developing cervical cancer in people with HPV. The reason for this is unclear, and the risk is small. However, the pill can help protect against other types of cancer, such as cancer of the uterus and ovarian cancer.
- Having a weakened immune system – the immune system helps rid the body of HPV. In some people, a weakened immune system can increase the risk of developing cervical cancer, so more frequent cervical screening tests may be needed. This includes people with human immunodeficiency virus (HIV) and those who have had an organ transplant.