The prostate
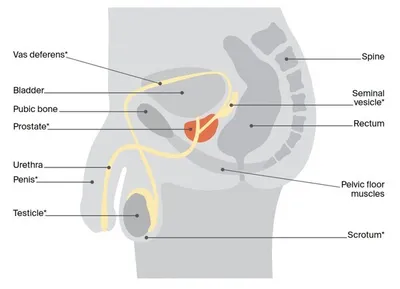
The prostate is a small gland about the size of a walnut.
It forms part of the male reproductive system. The prostate sits below the bladder and in front of the rectum (the end section of the large bowel).
Two glands called the seminal vesicles attach to the back of the prostate. The prostate is close to nerves, blood vessels, and muscles that help control erections and urination (the pelvic floor and urinary sphincter).
What the prostate does
The prostate produces fluid that helps to nourish and protect sperm. This fluid forms part of semen. Semen also contains sperm made in the testicles (testes) and fluid made by the seminal vesicles.
Urethra – This is a narrow tube that runs from the bladder and through the prostate to take urine (wee or pee) out of the body. The urethra also carries semen during ejaculation.
Ejaculation – When an orgasm occurs, millions of sperm from the testicles move through 2 tubes near the prostate called the vas deferens. The sperm then join with the fluids produced by the prostate and seminal vesicles to make semen. The muscle around the prostate contracts and pushes the semen into the urethra and out through the penis.
How the prostate grows
The main male sex hormone, testosterone, is made by the testicles and controls how the prostate grows. It is normal for the prostate to become larger with age. This may lead to a condition known as benign prostate hyperplasia or BPH.
Key questions
Answers to some key questions about prostate cancer are below.
What is prostate cancer?
Prostate cancer begins when abnormal cells in the prostate start growing in an uncontrolled way.
How common is it?
Prostate cancer is the most common cancer in Australian men (except for skin cancer). About 1 in 12 men will get prostate cancer by the age of 70, and 1 in 5 will get it in their lifetime. About 25,500 men are diagnosed each year, and rates are increasing. This may be in part because the population is growing and people may be living longer.
Anyone with a prostate can get prostate cancer – men, transgender women and intersex people. For information specific to you, speak to your doctor.
Non-cancerous changes to the prostate
A normal prostate often grows larger as you age and is called benign prostate hyperplasia (BPH). It is not usually due to cancer but BPH may press on the urethra and affect how you urinate (pee). You may:
- notice a weak stream of urine
- go to the toilet more often, especially at night
- need to pee urgently
- have trouble starting to pee
- dribble urine after peeing
- feel that the bladder is not empty.
Talk to your doctor if you have any of these urinary symptoms – because they can also happen in advanced prostate cancer.
What are the risk factors?
Factors that increase the risk of developing prostate cancer include:
- getting older – especially being aged 50 and over (more than 90% of people diagnosed with prostate cancer are aged 55 and over)
- family history of prostate, breast or ovarian cancer
- being of African or African-American descent.
While prostate cancer is less common if you are aged 50 and under, people aged 40 and over may have a higher than average risk of developing prostate cancer later in life if their prostate specific antigen (PSA) test results are higher than the typical range for their age.
Does prostate cancer run in families?
Having a strong family history of cancer increases the risk of developing prostate cancer. You may have inherited a gene that increases your risk of prostate cancer if you have:
- several close relatives on the same side of the family (can be your mother’s or father’s side) with prostate, breast and/or ovarian cancer, especially if due to a fault in the BRCA1 or BRCA2 genes
- a brother or father diagnosed with prostate cancer before the age of 60. In this case your risk is twice that of others.
If you are worried about your family history, talk to your general practitioner (GP). They may refer you to a family cancer clinic. For more information, call Cancer Council 13 11 20.
What screening test should I have?
Cancer screening is testing to look for cancer in people who don’t have any symptoms. The benefit of screening is that the cancer can be found and treated early. However, it is important that the benefits of screening outweigh any potential harms from treatment side effects. There is currently no national screening program for prostate cancer (national guidelines were under review when this information was last updated in May 2024).
The prostate specific antigen (PSA) blood test may identify fast-growing cancers that can spread to other parts of the body and would benefit from treatment. It may also find slow-growing cancers unlikely to be harmful, for which having treatment may cause significant side effects.
Some people without symptoms of prostate cancer choose to have regular PSA tests. It is important to talk to your doctor about the benefits and risks in your particular circumstances before having a PSA.
If you choose to have regular PSA tests, the current guidelines recommend that:
- men with no family history of prostate cancer have PSA testing every 2 years from age 50–69
- men with a family history of prostate cancer have PSA testing every 2 years starting from age 40–45 (depending on how strong the family history is) to age 69.
At-home PSA test kits are not recommended. The tests could be unreliable and do not come with qualified medical advice about the results.
A PSA screening test, requested by your doctor, should be available to you for free. Your doctor will also be able to explain what the results of your test mean, and can also refer you for other tests you may need.
For more information see Cancer Council Australia’s ‘Clinical Guidelines for PSA testing and early management of test-detected prostate cancer’.
Complementary or herbal supplements claiming to reduce PSA readings, or to prevent PSA from rising, are not recommended by Cancer Council. They may mask your true PSA, or cause you to have false results on medical pathology PSA testing.
What are the symptoms?
Early prostate cancer rarely causes symptoms. Even people diagnosed with advanced prostate cancer may have no symptoms. Difficulty passing urine is not always a symptom of prostate cancer, but you should see your doctor if you are worried or the following symptoms are ongoing:
- frequent or sudden need to urinate
- blood in the urine or semen
- a slow flow of urine
- needing to get up at night to pass urine
- feeling like your bladder is not empty after passing urine
- unexplained weight loss
- pain in bones, e.g. the neck, back, hips or pelvis.
Which health professionals will I see?
Your GP will arrange the first tests to assess your symptoms. If these tests do not rule out cancer, you will usually be referred to a specialist, who will arrange further tests.
Prostate cancer is usually diagnosed by a urologist, who will talk to you about your surgical or other options. You will usually also see a radiation oncologist to discuss radiation therapy. You may also be referred to a medical oncologist, who will discuss drug treatments. It’s important to find out all your options before making a decision.
Your specialists will discuss treatment options with other health professionals at what is known as a multidisciplinary team (MDT) meeting. During and after treatment, you will see a range of health professionals who specialise in different aspects of your care.
Health professionals you may see
- Gp – assists you with treatment decisions and works in partnership with your specialists in providing ongoing care; may monitor PSA levels and administer treatment
- Urologist – treats diseases of the urinary system and the male reproductive system, including prostate cancer; performs surgery
- Radiation Oncologist – treats cancer by prescribing and overseeing a course of radiation therapy
- Radiation therapist – plans and delivers radiation therapy
- Medical Oncologist – treats cancer with drug therapies such as chemotherapy, hormone therapy and targeted therapy (systemic treatment)
- Endocrinologist – diagnoses, treats and manages hormonal disorders, including osteoporosis
- Cancer care coordinator, prostate cancer specialist nurse – coordinate your care, liaise with MDT members, and support you throughout treatment; may be a clinical nurse consultant (CNC) or clinical nurse specialist (CNS)
- Nurse – administers drugs and provides care, information and support throughout management or treatment
- Nuclear medicine specialist – analyses bone scans and PET scans and delivers radionuclide therapies
- Radiologist – analyses x-rays and scans; an interventional radiologist may also perform a biopsy guided by ultrasound or CT, and deliver some treatments
- Pathologist – examines cells and tissue samples to determine the type and extent of the cancer
- Continence nurse – assesses bladder and bowel control, and helps you find ways to manage any changes
- Continence physiotherapist – provides exercises to help strengthen pelvic floor muscles and improve bladder and bowel control
- Exercise physiologist – prescribes exercise to help people with medical conditions improve their overall health, fitness, strength and energy level
- Occupational therapist – assists in adapting your living and working environment to help you resume your usual activities after treatment
- Sex therapist, sexual health physician – help you and your partner with sexuality issues before and after treatment; an erectile dysfunction specialist can give advice about erection problems
- Psychologist, counsellor, psychiatrist – help you manage your emotional response to diagnosis and treatment; may also help with emotional issues affecting sexuality
- Aboriginal and Torres Strait Islander liaison officer – if you identify as Aboriginal or Torres Strait Islander, supports you and your family during treatment and recovery
- Social worker – links you to support services and helps you with emotional, practical and financial issues
- Palliative care specialists and nurses – work closely with your GP and cancer team to help
control symptoms and maintain quality of life
How is prostate cancer diagnosed?
There is no simple test to find prostate cancer.
Two commonly used tests are the PSA blood test and the digital rectal examination. These tests, used separately or together, only show changes in the prostate. They do not diagnose prostate cancer. If either test shows an abnormality, you will usually have more tests.
Health professionals use Australian clinical guidelines to help decide when to use PSA testing and other early tests for prostate cancer.
Prostate specific antigen (PSA) blood test
Prostate specific antigen (PSA) is a protein made by both normal prostate cells and cancerous prostate cells. PSA is found in the blood and can be measured with a blood test. The test results will show the level of PSA in your blood as nanograms of PSA per millilitre (ng/mL) of blood.
There isn’t one normal PSA level for everyone. If your PSA level is above 3 ng/mL (called the threshold), this may be a sign of prostate cancer. But younger people or people who have a family history of prostate cancer may have a lower threshold. PSA levels can vary from day to day. If your PSA is higher than expected, your GP will usually repeat the test to help work out your risk of prostate cancer.
Your PSA level can be raised even when you don’t have cancer. Other common causes of raised PSA levels include benign prostate hyperplasia, recent sexual activity, an infection in the prostate, or a recent digital rectal examination. Some people with prostate cancer have normal PSA levels for their age range.
Free PSA or free-to-total test
Your doctor may also suggest that you have a free PSA test. This test measures the ratio of free PSA to total PSA in your blood. Free PSA is PSA that is not attached to other blood proteins. This test may be suggested if your PSA level is 4–10 ng/mL and your doctor is not sure whether you need a biopsy. A low free-to-total PSA ratio may be a sign of prostate cancer.
Digital rectal examination (DRE)
To do a digital rectal examination (DRE), the urologist places a finger into your rectum to feel the back of the prostate. They’ll wear gloves and put gel on their finger to make the examination more comfortable.
You may have further tests if the doctor feels a hard area or an odd shape. These changes do not always mean you have prostate cancer. Having a normal DRE also does not rule out prostate cancer, as the finger can’t reach all of the prostate and a DRE is unlikely to feel a small cancer.
GPs no longer regularly do DRE, although it may still happen depending on your PSA results and urinary symptoms. A urologist will usually do a DRE as part of looking at your prostate.
If your PSA is 3–10 ng/mL your doctor may suggest a DRE. If the DRE is normal and you have no symptoms, they may just do a repeat PSA test. If you are at high risk, they may suggest a urine biomarker test or MRI.
MRI scan
An MRI (magnetic resonance imaging) scan uses a powerful magnet and radio waves to build up detailed pictures of the inside of the body. A specialised MRI called mpMRI (multiparametric magnetic resonance imaging) is used if a doctor suspects prostate cancer. It combines the results of a number of MRI images to provide a more detailed image.
Your doctor may suggest an MRI to see if you need a biopsy or to guide the biopsy needle to a specific area of the prostate. It may also show if cancer has spread from the prostate to nearby areas.
Before the scan, let your medical team know if you have a pacemaker or any other metallic object in your body, as the magnet can interfere with some pacemakers. Newer pacemakers are often MRI-compatible.
Having an MRI – Sometimes a dye (called contrast) is injected into a vein before the scan to help make the pictures clearer. You will then lie on an examination table that slides into the scanner, which is a large metal cylinder open at both ends.
The scan is painless, but the scanner makes loud noises and is narrow, which makes some people feel anxious or claustrophobic. If you think you could become distressed, mention this beforehand to your medical team. You may be given a mild sedative to help you relax, or be able to bring someone into the room with you for support. You will have earplugs or headphones. The MRI scan may take around 30 minutes.
Medicare rebates for MRI scans to detect prostate cancer are only available if the MRI is ordered by a specialist and you meet certain conditions. You may still have to pay a gap fee.
Biopsy
Depending on the results of the MRI scan, your urologist may suggest a biopsy to remove tissue samples from the prostate. They will explain the risks and benefits of a prostate biopsy and give you time to decide if you want to have one. With specialised MRI scans available, your doctor may suggest you do not need a biopsy.
There are 2 main ways to perform a prostate biopsy, both of which are normally done under general anaesthetic:
- transperineal (TPUS or TPB) biopsy – a small ultrasound probe is inserted into your rectum. An image of the prostate appears on a screen and helps guide a needle which is inserted through the skin between the anus and the scrotum
- transrectal (TRUS) biopsy – the needle is inserted into the prostate via the rectum.
During either procedure, the doctor may take a number of samples from different areas of the prostate and also remove a sample from any suspicious areas seen on the MRI.
Side effects – Depending on the type of biopsy you have, after the procedure you may see a small amount of blood in your urine or bowel movements (poo) for a few days, and blood in your semen for a couple of months. After a TPUS biopsy, the risk of infection is extremely low. There is a greater risk of infection with a TRUS biopsy, but the risk is still low. Your doctor may suggest taking antibiotics before or after a biopsy if they think you may be at risk of infection.
The biopsy samples are sent to a laboratory, where a specialist doctor called a pathologist looks for cancer cells in the tissue. Waiting for the results can be stressful. For support, call Cancer Council 13 11 20.
Further tests
If the MRI or other biopsy results show prostate cancer, other tests may be done to work out whether the cancer has spread.
PSMA PET–CT scan
A PET (positron emission tomography) scan combined with a CT scan is a specialised imaging test. A PET–CT scan may be used to help detect cancers, or to find cancer that has spread or come back. The scan usually looks for a substance produced by prostate cancer cells called prostate specific membrane antigen (PSMA). Before the scan you will be injected with a small amount of a radioactive solution that makes PSMA show up on the scan. A Medicare rebate is available for newly diagnosed patients with intermediate or high-risk prostate cancer.
Bone scan
This scan can show if prostate cancer has spread to your bones. A tiny amount of radioactive dye is injected into a vein. You wait for a few hours while the dye moves through your bloodstream to your bones. The dye collects in areas of abnormal bone growth. Your body will then be scanned with a machine that detects the dye. A larger amount of dye will usually show up in any areas of bone with cancer cells. The scan is painless and the radioactive dye passes out of your body in a few hours.
CT scan
A CT (computerised tomography) scan uses x-rays to create detailed pictures of the inside of the body. A CT scan of the abdomen (belly) can show whether cancer has spread to lymph nodes in that area. A dye is injected into a vein to help make the scan pictures clearer. You will lie still on a table that moves slowly through the large, round doughnut shaped scanner. The scan itself takes a few minutes and is painless, but the preparation takes 10–30 minutes.
Which scan will I have?
A large clinical trial conducted in Australia, the proPSMA trial, showed that for certain men with newly diagnosed prostate cancer, a PSMA PET–CT scan is more accurate than having traditional CT and bone scans. A Medicare rebate was introduced in 2022, meaning about 75% of all newly diagnosed prostate cancer patients in Australia will be offered a PSMA PET–CT instead of a CT and bone scan.
Staging prostate cancer
The tests described above help your doctors work out if you have prostate cancer and whether it has spread. Working out how far the cancer has spread is called staging. It helps your doctors recommend the best treatment for you.
The most common staging system for prostate cancer is the TNM system. In this system, letters and numbers are used to describe the cancer, with higher numbers indicating larger size or spread.
TNM staging system
T stands for tumour - Refers to the size of the tumour (T0–4). T0 is smaller and T4 is larger.
N stands for nodes - N0 means the cancer has not spread to lymph nodes; N1 means it has spread to lymph nodes in the pelvis.
M stands for metastasis - M0 means the cancer has not spread outside of the pelvis; M1 means it has spread to lymph nodes, bone or other organs outside the pelvis.
Your doctor may also describe the cancer as:
- localised (early) – the cancer is contained inside the prostate
- locally advanced – the cancer is larger and has spread outside the prostate to nearby tissues or nearby organs such as the bladder, rectum or pelvic wall
- advanced (metastatic) – the cancer has spread to distant parts of the body such as the lymph nodes or bone. This is called prostate cancer even if the cancer is in a different part of the body.
Grading prostate cancer
The biopsy results will show the grade of the cancer. Grading describes how the cancer cells look under a microscope compared to normal cells.
For many years, the Gleason scoring system has been used to grade the tissue taken during a biopsy. If you have prostate cancer, you will have a Gleason score between 6 (slightly abnormal) and 10 (more abnormal). A newer system has been introduced to simplify the grading and make it easier to understand. Known as the International Society of Urological Pathologists (ISUP) Grade Group system, this grades prostate cancer from 1 (least aggressive) to 5 (most aggressive).
Risk of progression
Localised (early) prostate cancer is given a risk of progression that helps to guide treatment. The risk level is based on the size and grade of the cancer, and your PSA level before the biopsy:
- low risk – slow growing and not aggressive
- intermediate risk – likely to grow faster and be mildly to moderately aggressive
- high risk – likely to grow quickly and be more aggressive.
Localised (early) prostate cancer risk level
Risk level – low
- Gleason score = 6 or less
- ISUP grade group = 1
Risk level – intermediate
- Gleason score = 7
- ISUP grade group = 2-3
Risk level – high
- Gleason score = 8-10
- ISUP grade group = 4-5
Your PSA level and the tumour (T) size also help work out the cancer’s risk level.
Prognosis
Prognosis means the expected outcome of a disease. You can talk about your prognosis and treatment options with your doctor, but they can’t predict the exact course of the disease. They can give you an idea about the general outlook for people with the same type and stage of cancer.
To work out the stage, your doctor will consider your test results, the type of prostate cancer, the stage, grade and risk of progression, how well you respond to treatment, and your age, fitness and medical history.
Prostate cancer often grows slowly — even aggressive cases of prostate cancer tend to grow more slowly than other types of cancer. Some low-risk prostate cancers grow so slowly that they never cause any symptoms or spread; others don’t grow at all. Compared with other cancers, prostate cancer has one of the highest survival rates if diagnosed early.
The stage, grade and risk of progression of prostate cancer is complex, so ask your doctor to explain how it applies to you. Call Cancer Council 13 11 20 for information and support.
Management and treatment
There are different options for managing and treating prostate cancer, and more than one treatment may be suitable for you.
Your specialists will usually let you know your options. You may want to ask your treating doctor what other options are available to you. For example, if surgery is suggested you could ask if radiation therapy is also a suitable option. The treatment recommended by your doctors will depend on the stage and grade of the prostate cancer as well as your general health, age and preferences.
Management and treatment options by stage
- localised early
- active surveillance
- surgery and/or radiation therapy
- watchful waiting
- locally advanced
- surgery and/or radiation therapy
- androgen deprivation therapy (ADT) may also be suggested
- watchful waiting
- advanced (metastatic)
- usually androgen deprivation therapy (ADT)
- additional hormone therapy, newer drug therapy or targeted therapy is often combined with ADT
- sometimes chemotherapy or radiation therapy
- watchful waiting may be an option
- newer treatments as part of a clinical trial
Active surveillance
This is close monitoring of low-risk prostate cancer that isn’t causing symptoms. The aim is to avoid treatment that’s not yet needed, while watching for any changes that mean treatment should start.
Active surveillance is usually suggested for prostate cancers with a PSA level under 10 ng/mL, stage T1–2, and Gleason 6 or less (Grade Group 1). It may also be suggested for certain cancers with a PSA level between 10 and 20, and some Grade Group 2 cancers.
About 80% of Australians with low-risk prostate cancer choose active surveillance. It involves PSA tests every 3–6 months, as well as a digital rectal examination and mpMRI scans and biopsies as advised by your urologist. If results show the cancer is growing faster or more aggressively, your specialist may suggest starting active treatment.
Watchful waiting
Watchful waiting may be suggested if you are older and the cancer is unlikely to cause a problem in your lifetime. It may be an alternative to active treatment if the cancer is advanced at diagnosis, or if other health problems would make it hard to handle surgery or radiation therapy.
The aim of watchful waiting is to maintain quality of life rather than to treat the cancer. If the cancer spreads or causes symptoms, you will have treatment to relieve symptoms or slow the growth of the cancer, rather than to cure it.
Watchful waiting usually involves fewer tests than active surveillance. You will have regular PSA tests but probably won’t have a biopsy. Your doctor may suggest an MRI if your PSA is rising and of concern.
Surgery
For many people, surgery will be a suggested treatment option. It is worth discussing with your urologist or treating doctor whether there are other options, such as radiation therapy, available to you.
The main surgery for localised and locally advanced prostate cancer is a radical prostatectomy. It removes all the prostate, part of the urethra and the seminal vesicles. The urethra is rejoined to the bladder, and the vas deferens (that carry sperm from the testicles to the penis) will be sealed.
Some people have a nerve-sparing radical prostatectomy, to avoid damaging the nerves that control erections. This is only for lower-grade cancers where the cancer isn’t close to these nerves, and it works best for those who had strong erections before diagnosis. Problems with erections are common even with nerve-sparing surgery.
Cancer cells can spread from the prostate to nearby lymph nodes. For intermediate-risk or high-risk prostate cancer, nearby lymph nodes may also be removed (pelvic lymph node dissection).
How the surgery is done
There are different surgery methods to remove the prostate:
- open radical prostatectomy – usually done through one long cut in the lower abdomen (belly)
- laparoscopic radical prostatectomy (keyhole surgery) – small surgical instruments and a camera are inserted through several small cuts in the abdomen. The surgeon performs the procedure by moving the instruments using the image on the screen as a guide
- robotic-assisted radical prostatectomy – laparoscopic surgery performed with help from a robotic system. The surgeon uses a 3D picture and control panel to move robotic arms holding instruments.
Making decisions about surgery
Talk to your surgeon about whether surgery or another treatment such as radiation therapy is the best option for you. Also ask what surgical methods are available to you. Ask about the advantages and disadvantages of each option. There may be extra costs involved for some procedures and they are not all available at every hospital. You may want to consider getting a second opinion about the most suitable type of surgery.
The surgeon’s experience and skill are more important than the type of surgery offered. Compared to open surgery, both standard laparoscopic and robotic-assisted surgery usually mean a shorter stay in hospital, less bleeding, a smaller scar and a faster recovery. Current evidence suggests that the different approaches have a similar risk of side effects. Take the time you need to make the right decision for you.
What to expect after surgery
Recovery time – No matter which surgical method is used, a radical prostatectomy is major surgery and you will need time to recover. You can expect to return to your usual activities within about 6 weeks of the surgery. Usually you can start driving again in a couple of weeks, but heavy lifting should be avoided for 6 weeks.
Managing pain and discomfort – It’s common to have pain after the surgery, so you may need pain relief for a few days.
Having a catheter – You will have a thin, flexible tube (catheter) in your bladder to drain your urine into a bag. The catheter will be removed after 1–2 weeks once the wound has healed.
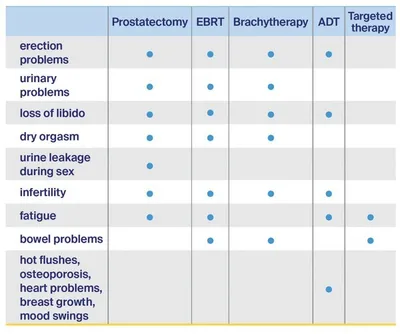
Side effects of prostate cancer surgery
You may experience some or all of the following side effects:
Nerve damage – The nerves needed for erections and the muscle that controls the flow of urine (sphincter) are both close to the prostate. It may be very difficult to avoid these during surgery, and any damage can cause problems with erections and bladder control. Sometimes the nerves will need to be removed to try to ensure all cancer is removed.
Loss of bladder control – You can expect to have some light dribbling or trouble controlling your bladder for some weeks to months after a radical prostatectomy. This is known as urinary incontinence or urinary leakage. You can use continence pads to manage urinary leakage. Bladder control usually improves in a few weeks and will continue to get better for up to a year after the surgery. In the long term, you might continue to have some light dribbling. Some people may consider having an operation to fix urinary incontinence. In rare cases, people have no control over their bladder.
Changes in erections – Problems getting and keeping erections after prostate surgery are common. This is often called erectile dysfunction (ED) or impotence. Erections may improve over months to a few years. It’s more likely you won’t get strong erections again if erections were already difficult before the operation.
Changes in ejaculation – During a radical prostatectomy, the tubes from the testicles (vas deferens) are sealed and the prostate and seminal vesicles are removed. This means semen is no longer ejaculated during orgasm (a dry orgasm). Your orgasm may feel different – in some cases it may be uncomfortable or, rarely, painful. A small amount of urine may leak during orgasm (which isn’t harmful to your partner).
Infertility – A radical prostatectomy will cause infertility and you will not be able to conceive a child without medical assistance. If you wish to have children, talk to your doctor before treatment about sperm banking or other options.
Changes in penis size – You may notice that your penis gradually becomes a little shorter after surgery. Talk to your doctor about whether vacuum erection devices and prescription medicines may help. A change to the size of your penis can be difficult to deal with.
Focal therapy
Focal therapy, also sometimes called ablation or focused therapy, uses high-intensity sound waves or targeted laser beams to target and destroy cancer cells.
This therapy is not a standard part of approved treatment guidelines and whether it works is unproven. Focal therapy may sometimes be offered as part of a clinical trial. Although this is not a new therapy, there have not been enough randomised clinical trials to confirm how well focal therapy works. You can still usually have other treatments afterwards if focal therapy does not work.
Radiation therapy
Also known as radiotherapy, radiation therapy uses a controlled dose of radiation to kill or damage cancer cells so they cannot grow, multiply or spread. Radiation therapy may be used:
- for localised or locally advanced prostate cancer – it has similar rates of success to surgery in controlling prostate cancer that has spread to the lymph nodes
- if you are not well enough for surgery or are older
- after a radical prostatectomy for locally advanced disease, if there are signs of cancer left behind or the cancer has returned where the prostate used to be
- for prostate cancer that has spread to other parts of the body
- for intermediate and high-risk prostate cancer, it is often combined with androgen deprivation therapy (ADT).
There are two main ways of delivering radiation therapy: from outside the body (external beam radiation therapy) or from inside the body (brachytherapy). You may have one of these types of radiation therapy, or you may have a combination of both.
External beam radiation therapy (EBRT)
In EBRT, a machine precisely directs radiation beams to the prostate. Each treatment session takes about 15 minutes. You will lie on the treatment table under the radiation machine. The machine doesn’t touch you but may rotate around you. You can’t see or feel the radiation.
There are different types of EBRT. Your radiation oncologist will talk to you about the most suitable type for your situation. Usually, EBRT for prostate cancer is given Monday to Friday for 4–9 weeks. Some newer forms of EBRT are given in 5–7 treatments over 2 weeks.
EBRT does not make you radioactive and there is no danger to people near you. Most people feel well enough to work and do their normal activities, though fatigue may increase as your treatment continues.
Reducing the risk of bowel side effects
Radiation therapy can cause bowel changes.
- To move the bowel away from the prostate and help prevent side effects, the radiation oncologist may suggest a spacer. Before treatment begins, a temporary gel or balloon is injected between the prostate and bowel. This is done by a urologist as a day procedure under a light anaesthetic. The cost of a spacer is not subsidised by Medicare. Ask your doctors what you will have to pay and the benefits for your situation.
- The radiation therapist may advise you to drink fluids before each treatment session so you have a full bladder. This will expand your bladder and push the bowel higher up into the abdomen, away from the radiation.
- The radiation team may also advise you to go to the toilet to empty your bowels before each treatment. This can help to ensure the prostate is in the same position every time.
Internal radiation therapy (brachytherapy)
Brachytherapy is a type of targeted internal radiation therapy where the radiation source is placed inside the body near the prostate. Giving doses of radiation directly into the prostate can lower the amount of unwanted radiation going into areas such as the rectum and bladder.
There are 2 different types of brachytherapy: permanent and temporary. If you already have significant urinary symptoms or a large prostate, brachytherapy may not be suitable.
Safety precautions after brachytherapy
If you have permanent brachytherapy your body may give off some radiation for a period of time. The levels will gradually fall over a number of months. This radiation only travels a short distance, which means there is little radiation outside your body.
You will still need to take care spending time in close contact with pregnant women and young children for a few weeks or months after the seeds are inserted. Your treatment team will explain the precautions to you. You should use a condom during sex (intercourse and oral) for this precaution time in case a seed comes out (this is rare).
If you have temporary brachytherapy, you will not be radioactive once the wires are removed after treatment, and there is no risk to other people and no special precautions are needed during sex.
How brachytherapy is done
Permanent brachytherapy (seeds)
- Also called low-dose-rate (LDR) brachytherapy.
- Most suitable for people with few urinary symptoms, and small cancers with a low PSA level (less than 10) and a low to intermediate Gleason score or Grade Group.
- Multiple radioactive metal “seeds”, each about the size of a grain of rice, are put into the prostate under a general anaesthetic.
- The radiation oncologist uses needles to insert the seeds through the skin between the scrotum and anus (perineum). Ultrasound is used to guide the seeds into place.
- The procedure takes 1–2 hours and you can usually go home the same or next day.
- The seeds slowly release radiation into the area of the prostate to kill cancer cells.
- There are safety issues for patients and others.
- The seeds lose their radioactivity after about a year. They are not removed from the prostate.
Temporary brachytherapy
- Also called high-dose-rate (HDR) brachytherapy.
- May be offered to people with a higher PSA level and a higher Gleason score or Grade Group. It is often given with a short course of EBRT.
- The radiation is delivered through hollow needles that are inserted into the prostate while you are under anaesthetic.
- The needle implants stay in place for several hours or, in some cases, overnight. You usually will have 1–3 brachytherapy treatments during this time.
- For each treatment, radioactive wires will be inserted into the needles to deliver a high dose of radiation to the prostate in a few minutes.
- The needle implants are taken out after the final radiation dose is delivered. You will have no
radiation left in your body. - There are no safety issues.
- In some cases, the implant procedure is repeated 1–2 weeks later.
Side effects of radiation therapy
The side effects you experience will vary depending on the type and dose of radiation, and the areas treated. You may experience some of the following side effects. Most side effects are temporary and tend to improve gradually in the weeks after treatment ends, though some may continue for longer. Some side effects may not show up until many months or years after treatment. These are known as late effects. Talk to your doctor or treatment team about ways to manage any side effects you have.
Short-term side effects
Fatigue – The effects of radiation on your body may mean you become tired during treatment. Fatigue may build up during treatment and usually improves 1–2 months after treatment ends, but occasionally can last up to 3 months.
Urinary problems – Radiation therapy can irritate the lining of the bladder and the urethra. This is known as radiation cystitis. You may pass urine more often or with more urgency, have a burning feeling when urinating or a slower flow of urine. If you had urinary issues before treatment, you may be more likely to have issues with urine flow. If you see blood in the urine, tell your doctor as this may need treatment. If you are unable to empty your bladder (urinate) right after brachytherapy, you may need a catheter for a few days or weeks.
Bowel changes – Radiation therapy can irritate the lining of the bowel and rectum. You may have smaller and more frequent bowel movements, need to go to the toilet quickly, or feel that you can’t completely empty the bowel. Less commonly, there may be some blood in the faeces (poo or stools). If this happens, let your doctor know as there are treatments that can stop the bleeding.
Ejaculation changes – You may notice that you feel the sensation of orgasm but ejaculate less or no semen after radiation therapy. This is known as dry orgasm, which may be a short-term or permanent side effect. In some rare cases, you may experience pain when ejaculating. The pain usually eases over a few months.
Long-term or late effects
Infertility – Radiation therapy to the prostate usually causes infertility. If you might want to have children, speak to your doctor before treatment about sperm banking or other options.
Urinary problems – Bladder changes, such as frequent or painful urination, can appear months or years after treatment. After brachytherapy, scarring can develop around the urethra, which can block the flow of urine. This can usually be repaired. It is important to let your doctor know if you have any problems with urinating or notice any bleeding.
Bowel changes – Bowel changes, such as diarrhoea, wind or constipation, can appear months or years after treatment. Bleeding from the rectum can also occur. In rare cases, there may be loss of bowel control (faecal incontinence) or blockage of the bowel. It is important to let your doctor know about any bleeding, or if you have pain in the abdomen and difficulty opening your bowels.
Erection problems – Radiation may damage the nerves and blood vessels that control erections. This can make it difficult to get and keep an erection, especially if you have had problems before treatment. Having ADT can also cause problems with erections. Erection problems may take time to appear and can be ongoing or permanent.
Androgen deprivation therapy (ADT)
Prostate cancer needs testosterone to grow. Reducing how much testosterone your body makes may slow the cancer’s growth or shrink the cancer temporarily. Testosterone is an androgen (male sex hormone made by the testicles), so this treatment is called androgen deprivation therapy (ADT). It is also known as hormone therapy.
ADT for locally advanced cancer may be used after a radical prostatectomy or with radiation therapy. It may also be given to help control advanced prostate cancer. There are different types of ADT:
ADT injections – The most common form of ADT involves injecting a drug to block the production of testosterone. Your GP or specialist can give the injections. How often you have injections depends on the type of ADT. They may be given monthly, every 3 months or every 6 months. ADT injections can help slow the cancer’s growth for years.
ADT injections may also be used before, during and after radiation therapy to increase the chance of getting rid of the cancer. They are sometimes combined with chemotherapy.
Intermittent ADT – Occasionally ADT injections are given in cycles and continue until your PSA level is low. Injections can be restarted if your PSA rises again. This is known as intermittent ADT. In some cases, this can reduce side effects. It is not suitable for everyone.
Anti-androgen tablets – Often called hormone tablets, anti-androgen tablets may be given in combination with ADT injections.
Removing the testicle/s (orchidectomy) – This surgery is an uncommon way to lower how much testosterone your body makes.
If you have advanced prostate cancer, you may choose to have surgery rather than regular ADT injections or tablets.
Surgery to remove both testicles is called a bilateral orchidectomy. It is possible to have a silicone prosthesis put into the scrotum to keep its shape. Removing only the inner part of the testicles (subcapsular orchidectomy) also lowers testosterone and does not need a prosthesis.
Side effects of ADT
ADT may cause side effects because of the lower levels of testosterone in the body. Side effects may include:
- tiredness that doesn’t go away with rest (fatigue)
- reduced sex drive (low libido)
- difficulty getting an erection (impotence)
- shrinking of the testicles and penis
- loss of muscle strength
- hot flushes and sweating
- weight gain, especially around the middle
- breast swelling and tenderness
- mood swings, depression, trouble with thinking and memory
- loss of bone density (osteoporosis) – calcium and vitamin D supplements and regular exercise help reduce the risk of osteoporosis
- higher risk of diabetes, high cholesterol and heart disease – more likely the longer you have ADT. Ask your doctor about these risks.
Adjusting to changes in your testosterone levels takes time.
To find out more about ADT, visit the Prostate Cancer Foundation of Australia or call them
on 1800 22 00 99. For information about erectile and other sexual health issues, visit the Healthy Male.
Advanced prostate cancer treatment
If prostate cancer has spread (metastasised) to other parts of the body, you may have a combination of drug therapies, EBRT, ADT or chemotherapy.
Drug therapies
Newer drug therapies may be used to treat advanced prostate cancer that has come back while having ADT. These drugs (e.g. abiraterone, apalutamide, darolutamide, enzalutamide) are often hormone therapy tablets that can be combined with ADT to help control the cancer and reduce symptoms. They are usually taken daily.
These new drugs are available through the PBS for advanced prostate cancer. Treatment usually aims to relieve symptoms or keep the cancer under control for years. Hormone- sensitive prostate cancer may be treated with ADT alongside other treatments outlined below. Using drug therapies, chemotherapy and hormone therapies together is often called triple therapy.
Other drug therapies include drugs that target specific features of cancer cells, called targeted therapy. These drugs (e.g. olaparib) are used for cancer with gene changes (such as BRCA) linked to prostate cancer.
Listen to our podcast episode ‘New Cancer Treatments’
Radiation therapy
You may be offered radiation therapy to slow the growth of the cancer. Radiation therapy may be given to the areas where the cancer has spread, such as the lymph nodes or bones. You may also have radiation therapy to the prostate if you have not previously had any radiation treatment.
Download our booklet ‘Understanding Radiation Therapy’
Chemotherapy
Chemotherapy uses drugs to kill cancer cells or slow their growth. If the prostate cancer continues to spread despite using ADT and other drug therapies, chemotherapy may be suitable. Chemotherapy may also be offered as part of initial treatment in combination with ADT.
Generally, chemotherapy is given through a drip (infusion) into a vein (intravenously). For prostate cancer, chemotherapy is usually given once every 3 weeks for 4–6 months and you do not stay in hospital.
Side effects of chemotherapy may include fatigue, hair loss, changes in blood counts increasing the risk of bleeding or infections, numbness or tingling in the hands or feet (peripheral neuropathy), changes in nails, watery eyes and runny nose, and rare side effects, such as allergic reactions or blocked tear ducts.
Download our booklet ‘Understanding Chemotherapy’
Transurethral resection of the prostate (TURP)
This surgical procedure is used to treat problems passing urine. It helps with symptoms of more advanced prostate cancer, such as the need to pass urine more often and a slow flow of urine.
If you have localised cancer, TURP may be used before radiation therapy to relieve symptoms of urinary blockage. TURP is also used to treat benign prostate hyperplasia.
You will be given a general or spinal anaesthetic. A narrow tube-like instrument is passed through the opening of the penis and up the urethra to remove the blockage. The surgery takes about an hour, and you will usually stay in hospital for a couple of days. Side effects may include blood in urine or problems urinating for a few days.
Bone therapies
If the prostate cancer has spread to the bones (bone metastases), your doctor may suggest treatments to manage the effect on the bones. Drugs can be used to prevent or minimise bone pain and reduce the risk of fractures and pressure on the spinal cord.
Radiation therapy can also be used to control bone pain, to prevent fractures or help them heal, and to treat pressure on spinal nerves (spinal cord compression) from cancer that has spread to the spine.
Palliative treatment
Palliative treatment helps to improve quality of life by managing the symptoms of cancer without trying to cure the disease. It is about living for as long as possible in the most satisfying way you can.
As well as slowing the spread of cancer, palliative treatment can relieve pain and help manage other symptoms. Treatment may include:
- radiation therapy to control pain if the cancer has spread to the bones
- pain medicines (analgesics)
- radionuclide therapy to control pain and improve quality of life. This involves swallowing or being injected with radioactive material which spreads through the body and targets cancer cells. The high doses of radiation kill cancer cells with little damage to normal tissues.
Palliative treatment is part of palliative care, in which a team of health professionals aims to meet your physical, emotional, practical, cultural, social and spiritual needs. They also support families and carers.
Download our booklet ‘Living with Advanced Cancer’
Download our booklet ‘Understanding Palliative Care’
Download our booklet ‘Understanding Cancer Pain’
For more information or support, call Cancer Council 13 11 20.
Managing side effects
It will take some time to recover from the physical and emotional changes caused by treatment for prostate cancer.
Treatment side effects can vary – some people experience many side effects, while others have few. Side effects may last from a few weeks to a few months or, in some cases, years or permanently. Fortunately, there are many ways to reduce or manage side effects.
Side effects you may experience
Erection problems
You may have trouble getting or keeping an erection firm enough for intercourse (vaginal or anal) or other sexual activity after any treatment for prostate cancer. This is called erectile dysfunction or impotence.
The prostate is close to nerves, muscles and blood vessels that help control erections. These can be damaged during treatment. If the nerves are removed during surgery, erection problems happen immediately. After radiation therapy and ADT, problems may begin slowly.
The quality of your erections usually improves over time and can continue to improve for up to 3 years after treatment has finished. However, sometimes erection problems may be permanent.
Aside from cancer treatment, erection problems become more common with age. Erections can also be affected by diabetes and heart disease; some medicines for blood pressure or depression; surgery to the bowel or abdomen; smoking or heavy drinking; or emotional concerns.
Before and after treatment, you can help keep your penis healthy (penile rehabilitation) in various ways. These may include:
- foreplay and other sexual intimacy with a partner or masturbating
- trying to get erections, starting a month after surgery
- taking prescribed medicines to maintain blood flow in the penis
- stopping smoking and limiting the amount of alcohol you drink
- doing pelvic floor exercises
- injecting prescribed medicine into the penis.
Even without a full erection, you can still reach orgasm by stimulating the penis.
Ways to improve erections
There are several medical options to try to improve the quality of your erections, no matter what type of prostate cancer treatment you have had. Ask your treatment team for more details about these methods and other things you can do to improve erections.
Tablets
Your doctor can prescribe tablets to increase blood flow to the penis. These only help if the nerves controlling erections are working. These tablets should not be taken with certain blood
pressure medicines. Check with your doctor about the medicines you take.
Your doctor may recommend using the tablets before and soon after surgery, as the increased blood flow can help preserve penis health until the nerves recover. Tablets are also an option after radiation therapy and ADT.
Vacuum erection device (VED)
A vacuum erection device (VED) or “penis pump” uses suction to make blood flow into the penis. This device can also help to strengthen or maintain a natural erection. Talk to your doctor about suitable devices for you and where to buy them.
You place a clear, rigid tube over the penis. A manual or battery-operated pump then creates a vacuum that causes blood to flow into the penis so it gets hard. You place a rubber ring at the base of the penis to keep the erection firm for intercourse after the pump is removed. The ring can be worn comfortably for 30 minutes.
Penile injection therapy (PIT)
Penile injection therapy (PIT) involves injecting the penis with medicine that makes blood vessels in the penis expand and fill with blood, creating an erection. This usually occurs within 15 minutes and lasts for 30–60 minutes.
The medicine has to be prescribed by a doctor. It often comes in pre-loaded syringes, which are single use. You can also buy it in vials from a compounding pharmacy and measure it out into a syringe yourself.
You will be taught how to inject the penis. Injecting your penis may sound unpleasant, but many people say it causes only a moment of discomfort.
PIT works well for many people, but a few may have pain and scarring. A rare side effect is a prolonged and painful erection (priapism). This needs emergency medical attention.
Implants
A penile prosthesis is a permanent implant that allows you to create an erection. Flexible rods or thin, inflatable cylinders are placed in the penis during surgery and connected to a pump in the scrotum. You turn on or squeeze the pump when you want an erection.
An implant is not usually recommended for at least a year after prostate cancer treatment, and non-surgical options such as oral medicines or injections will usually be tried first.
Occasionally, penile implants need to be removed. If this happens, you will no longer be able to have an erection.
You may see or hear ads for ways to treat erection problems. These ads may be for herbal preparations, natural therapies, nasal sprays and lozenges. If you are thinking about using these products, talk to your doctor first, as there could be risks without any benefits. Products that contain testosterone or act like testosterone in the body may encourage some cancers to grow.
Urinary problems
Trouble controlling the flow of urine (urinary incontinence) is a common side effect of some treatments for prostate cancer.
After prostate surgery, issues with urinary incontinence are common for several weeks or months and usually improve slowly over time. Most people will need to use incontinence pads in the first few weeks after surgery. Only a small number of people will need to use incontinence pads long term. You may find that you:
- lose a few drops of urine when you cough, sneeze, strain or lift something heavy
- leak some urine during sex
- have blood in your urine that may last a few weeks.
Urinary problems caused by radiation therapy are usually temporary and tend to improve within a few months of finishing treatment. In some cases, radiation therapy can:
- reduce how much urine the bladder can store
- irritate the bladder
- narrow the urethra
- weaken the pelvic floor muscles.
You may also find that you need to pass urine more often or in a hurry, or that you have difficulty passing urine. Sometimes, medicines or surgery can improve urine flow – ask your doctor if this is an option for you.
If you have ongoing side effects after cancer treatment, talk to your GP about developing a GP Management Plan and Team Care Arrangement to help you manage them. This means you may be eligible for a Medicare rebate for up to 5 visits each calendar year to allied health professionals.
Coping with urinary incontinence
- Start pelvic floor exercises before surgery to help reduce the likelihood of ongoing urinary
incontinence after surgery. The exercises are also important after surgery. - Ask your doctor, urologist, continence physiotherapist or continence nurse about how to correctly do pelvic floor exercises.
- Drink plenty of water to dilute your urine – concentrated urine can irritate the bladder.
- Keep drinking plenty of fluids, even if you are afraid of leakage. Dehydration can cause constipation, which may also lead to leakage and difficulty passing urine.
- Limit tea and coffee as they contain caffeine, which can irritate the bladder. Alcohol and carbonated drinks may also irritate the bladder.
- Talk to a continence nurse or continence physiotherapist about continence products if needed. These include absorbent pads to wear in your underpants, and bed and chair covers. They may also recommend medicines or a special plastic clamp for your penis.
- Ask your continence nurse or GP if you can apply for the Continence Aids Payment Scheme. This is a yearly payment to help cover the cost of continence products.
- If incontinence does not improve after 6–12 months, talk to your doctor or urologist about whether surgery is an option. For example, a surgically inserted sling or artificial sphincter works by pulling the urethra up to help the sphincter muscle close more effectively.
- Get resources from the Prostate Cancer Foundation of Australia or call them on
1800 22 00 99 and the Continence Foundation of Australia or phone 1800 33 00 66.
Download our booklet ‘Exercise for People Living with Cancer’
Other changes to your sexual function
Changes may affect your sex life, feelings of pleasure and intimacy.
Loss of libido – Reduced interest in sex (low libido) is common during cancer treatment. While anxiety and fatigue can affect libido, it can also be affected by ADT, which lowers testosterone levels, and by the sexual side effects associated with radiation therapy or surgery. Sex drive usually returns when treatment ends, but sometimes changes in libido are ongoing.
Loss of pleasure from prostate stimulation – Depending on whether the prostate is removed, or radiation or hormone treatment damages the prostate, you may no longer feel pleasure from the prostate being stimulated. Consider other ways to feel pleasure, such as stimulating the penis or the area around the anus.
Dry orgasm – After surgery, you will feel the muscular spasms and pleasure of an orgasm, but you won’t ejaculate semen. This is called a dry orgasm. It happens because the prostate and seminal vesicles that produce semen are removed during surgery, and the tubes from the testicles (vas deferens) are sealed. Radiation therapy may also affect how much sperm you make, but this is often temporary.
Leaking urine during sex – A radical prostatectomy can weaken the sphincter muscle that controls the flow of urine. This may cause a little urine to leak during intercourse and orgasm. You may find this embarrassing, but it won’t harm your partner. Before sex, empty your bladder. Try sex in the shower, or use a condom or a constriction ring (available from sex shops) at the base of the penis to prevent leakage. Talk to your doctor if you are concerned.
Managing changes in your sex life
- Talk about the changes and your feelings about sex. If you have a partner, changes may affect you both. Reassure them that intimacy is still possible and important to you.
- Focus on giving and receiving pleasure in different ways without sexual penetration. Other ways of expressing love include touching, holding, caressing and massage.
- Try adult products (e.g. sex toys, dildos, vibrators) to spark interest in sex. Your partner can satisfy themselves, either alone or with you present.
- Take time to get used to any changes. Look at yourself naked in the mirror and touch your genitals to feel any differences or soreness.
- Start slowly – touch each other’s skin, then genitals.
- When you feel ready, try vaginal intercourse even with a partial erection. This may encourage more and better erections. A partial erection may not be strong enough for anal sex but you could work up to this using stimulation to encourage stronger erections.
- Explore and understand any changes by masturbating.
- Ask your partner to help you reach orgasm through gentle hand-stroking. Use silicone-based lubricants for prolonged stimulation.
- Try different positions to find what feels comfortable. Kneeling or standing may also help with erections.
- Mindfulness techniques may help you stay in the moment. Listen to our ‘Finding Calm During Cancer’ podcast for exercises.
- Talk to your doctor, a sexual health physician or counsellor if the changes are causing depression or relationship problems.
- Download the Prostate Cancer Foundation of Australia’s booklet ‘Understanding Sexual issues following prostate cancer treatment’
Restoring your sex life
Prostate cancer can affect your sex life physically and emotionally. How much will depend on factors such as the cancer treatment and its side effects, your general health, how you and your partner/s communicate, and your self-confidence. It takes time to adjust to changes in your sex drive, your self-esteem and relationships.
Telling a new partner
Deciding when to tell a potential sexual partner about your cancer experience isn’t easy, and you may even avoid dating or sex. It can be helpful to wait until you and your new partner have developed a mutual level of trust and caring. You might prefer to talk with a new partner about your concerns before becoming sexually intimate. By communicating openly, you avoid misunderstandings and may find that your partner is more accepting and supportive.
Fertility problems
Infertility is common after surgery, radiation therapy or ADT for prostate cancer. This means you can no longer have children naturally. If you may want to have children in the future, you (and a partner if you have one) should talk to your doctor about the options before treatment starts. You may be able to store some sperm at a fertility clinic to use when you are ready to start a family.
Radiation therapy may affect sperm quality for 6–12 months after treatment and cause birth defects. You will need to use contraception or not have sexual intercourse to avoid conceiving during this time.
Other side effects
Treatment for prostate cancer may lead to a range of other concerns, but most of these can be managed.
Fatigue – Cancer treatment often makes people very tired. After surgery, it may take some time to get back your strength. With external beam radiation therapy, you may get particularly tired near the end of treatment and for some weeks or months afterwards. Regular exercise can help reduce tiredness.
Download our fact sheet ‘Fatigue and Cancer’
Bowel problems – Although this is an uncommon side effect of radiation therapy, you may experience rectal bleeding after treatment. It is common to have a stronger sensation of needing to have a bowel movement. A gastroenterologist or colorectal surgeon may treat ongoing bowel problems with changes to your diet, steroid suppositories (a tablet that you insert into the rectum through the anus), laser therapy or other treatments applied to the bowel wall. For more information, talk to your radiation oncologist or a continence nurse.
Hot flushes – You may experience hot flushes if you are having ADT. Things that may help include drinking less alcohol, avoiding hot drinks, wearing loose-fitting cotton clothing, getting regular exercise, learning relaxation techniques, and trying acupuncture. For more information, talk to your doctor.
Osteoporosis – Loss of bone density can be a delayed side effect of ADT, so your specialist or GP may need to monitor your bone mineral density. Regular weight-bearing exercise (e.g. brisk walking, light weights or a guided exercise program), eating calcium-rich foods (e.g. yoghurt, milk, tofu, green vegetables), getting enough vitamin D, limiting how much alcohol you drink, and not smoking will also help keep your bones strong. For more information, visit Healthy Bones Australia or call them on 1800 242 141.
Heart problems – Because ADT can increase the risk of heart problems and stroke, your doctor will monitor how well your heart is working.
Loss of muscle mass and strength – You may find a decrease in muscle mass the longer you are on ADT. So staying as fit and active as you can may help. Clinical trials are looking at how strength and resistance training (used with supplements) may preserve muscle mass for people with prostate cancer.
Hormone effects – Weight gain, mood swings, breast swelling, body changes, and high cholesterol are more likely to happen the longer you use ADT.
How exercise and diet can help
Regular exercise can help manage the side effects of ADT. It improves mood, heart health, bone and muscle strength, and energy levels.
Whatever your age or fitness level, a physiotherapist or exercise physiologist can develop an exercise program to meet your specific needs. Ask your doctor for a referral. Our ‘Exercise for People Living with Cancer’ booklet includes examples of different cardio and aerobic exercise, strength and resistance training and flexibility exercises.
ADT can lead to weight gain and increase the risk of high cholesterol. Aim to eat a balanced diet with a variety of fruit, vegetables, wholegrains and protein-rich foods. It may help to see a dietitian.
Life after treatment
For most people, the cancer experience doesn’t end on the last day of treatment.
Life after cancer treatment can present its own challenges. You may have mixed feelings when treatment ends and worry that every ache and pain means the cancer is coming back.
Some people say that they feel pressure to return to “normal life”. It is important to allow yourself time to adjust to the physical and emotional changes, and establish a new daily routine at your own pace. Your family and friends may also need time to adjust.
Cancer Council 13 11 20 can help you connect with other people who have had prostate cancer, and provide you with information about the emotional and practical aspects of living well after cancer.
Follow-up appointments
After treatment ends, you will have regular appointments to monitor your health, manage any long-term side effects, check that the cancer hasn’t come back, and discuss any concerns you have. During check-ups, you may have a physical examination, x-rays or scans, and a PSA test.
Depending on the type of treatment you had, PSA results will vary:
- After surgery, if it has been possible to remove all of the cancer, there should be no prostate cells left to make PSA antigen and your PSA level should drop quickly.
- After radiation therapy, your PSA level will drop gradually and it may take 2–3 years for your PSA to reach its lowest level.
- If you have ADT as well as radiation therapy, your PSA level will generally be very low while undergoing treatment.
The usefulness of the PSA test will vary. If you had localised prostate cancer, it can help find any cancer cells that come back. With advanced prostate cancer, particularly when the Gleason score or Grade Group is very high, the PSA test may be less useful. Your doctor will also consider your symptoms and other test results along with the PSA test results. These all help to build a picture of what is happening to the cancer that is more accurate and informative than the PSA test alone.
Talk to your doctor about how often you will need to have check-ups or a PSA test. Over time, if there are no further problems, you will have check-ups less frequently. If you notice any new symptoms between check-ups, you should let your GP or specialist know immediately.
When a follow-up appointment or test is approaching, many people find that they think more about the cancer and may feel anxious. Talk to your treatment team or call Cancer Council 13 11 20 if you are finding it hard to manage this anxiety.
If you have had localised prostate cancer, you can make a free online survivorship care plan (SCP). The plan suggests linking your doctors and other care providers, and offers information on common side effects and treatments you have had.
What if cancer returns?
Sometimes prostate cancer does come back after treatment, which is known as a recurrence. If your PSA level starts to rise and the cancer has not spread beyond the prostate, this may mean you still have cancer cells in the prostate area. If this happens, you may be monitored with regular blood tests or you may be offered further treatment, which is known as salvage treatment.
Your options will depend on the treatment you had. If you had surgery, you may be offered radiation therapy. If you had radiation therapy, some people may be offered further radiation therapy, while others may have the option of surgery or other treatments. If the cancer has spread beyond the prostate, ADT is usually suggested and sometimes radiation therapy. Surgery may be an option in some cases. You may be offered palliative treatment to manage symptoms.
It is possible for the cancer to come back in another part of your body. In this case, you may have treatment that focuses on the area where the cancer has returned. Talk to your doctors about the options. You can also call Cancer Council 13 11 20 for more information.
How you might feel
It is natural to have a wide variety of emotions after a cancer diagnosis and during treatment, including anger, fear, anxiety, sadness and resentment. Feelings may increase over time as you adjust to the physical side effects of treatment.
Everyone has their own ways of coping. Give yourself and those around you time to deal with the emotions that cancer can cause. For support, call Cancer Council 13 11 20.
If you have continued feelings of sadness, have trouble getting up in the morning or don’t feel like doing things that previously gave you pleasure, you may be depressed. This is quite common during cancer.
If your emotions are affecting your day-to-day life, talk to your GP. Counselling or medication – even for a short time – may help. Some people can get a Medicare rebate for sessions with a psychologist. Cancer Council SA also provides a free counselling program. Visit Beyond Blue or call them on 1300 22 4636 for information about depression and anxiety. For 24-hour crisis support, visit Lifeline or phone 13 11 14.