The bones
Bones have a number of important functions.
These include:
- supporting the body
- protecting internal organs
- attaching to muscles to allow movement
- containing bone marrow, which stores and produces new blood cells
- storing proteins, minerals and nutrients, such as calcium.
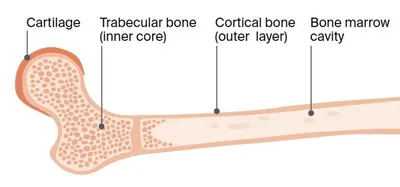
Bones are made up of different parts, including a hard, outer layer (known as cortical or compact bone) and a spongy inner core (known as trabecular or cancellous bone). Bone marrow – a substance
containing fat and blood stem cells that can become red blood cells, white blood cells, or platelets – is
found in this spongy core.
Normal bone is constantly going through a process called remodelling, or turnover, in which old bone is broken down and replaced with new bone.
Bone structure
Bones are made up of a hard outer layer, an inner core, and spongy bone marrow found in this inner core. Cartilage is the tough material at the end of each bone that allows one bone to move against another at a joint.
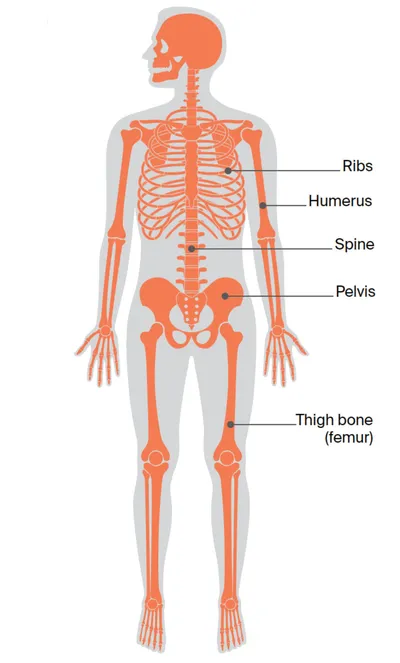
Bones of the body
Cancer can spread to any bone in the body. Bones commonly affected include the spine, ribs, pelvis and upper bones of the arms and legs.
Key questions
Answers to some key questions about secondary bone cancer are below.
What is secondary bone cancer?
Secondary bone cancer means that the cancer started in another part of the body, and has now spread (metastasised) to the bone.
Secondary cancer in the bone, also called bone metastases or bone mets, often keeps the name of the original cancer. For example, breast cancer that has spread to the bone may be called secondary or metastatic breast cancer. Because the cancer has spread, it is considered advanced or stage 4 cancer.
Cancer cells can spread from the original cancer (the primary cancer), through the bloodstream or lymph vessels, to any of the bones in the body. Bones commonly affected by secondary bone cancer include the spine, ribs, pelvis, and upper bones of the arms (humerus) and legs (femur).
Which cancers spread to the bone?
Any type of cancer can spread to the bone. The cancers most likely to spread to the bone include:
- prostate cancer
- breast cancer
- lung cancer
- kidney cancer
- thyroid cancer
- myeloma (a type of blood cancer)
- melanoma.
What types of secondary bone cancer are there?
There are 2 main types of secondary bone cancer. Osteolytic is where bone is broken down by the cancer cells without being replaced by new bone. Holes, also called lytic lesions, might form in the bone, which increases the risk of a break or fracture.
Osteoblastic bone cancer is where new bone cells form abnormally in some areas. These areas are called osteoblastic (or sclerotic) lesions and even though they are very hard (dense), they make the bone weak and deformed.
Most people with secondary bone cancer develop either osteolytic or osteoblastic changes, but some have both.
What types of secondary bone cancer are there?
There are 2 main types of secondary bone cancer. Osteolytic is where bone is broken down by the cancer cells without being replaced by new bone. Holes, also called lytic lesions, might form in the bone, which increases the risk of a break or fracture.
Osteoblastic bone cancer is where new bone cells form abnormally in some areas. These areas are called osteoblastic (or sclerotic) lesions and even though they are very hard (dense), they make the bone weak and deformed.
Most people with secondary bone cancer develop either osteolytic or osteoblastic changes, but some have both.
How common is it?
Secondary bone cancer is much more common than primary bone cancer in Australia. It is more common in adults than children. The bone is one of the most common places cancer may spread to, along with the lymph nodes, liver, lungs and brain.
What are the signs and symptoms?
These are some signs and symptoms of secondary bone cancer. If you notice any of these symptoms, see your doctor.
Bone pain – This is often the first and most common symptom. The pain may be a dull, persistent ache. It can get worse with movement and is often worse at night.
Fractures – Cancer cells can weaken the bones and cause them to break more easily, often with little or no force (this is known as a pathological fracture).
High calcium levels in the blood (hypercalcaemia) – As the bone breaks down, calcium is released into the bloodstream. When calcium builds up in the blood, it may cause severe tiredness (fatigue), a feeling of sickness (nausea), vomiting, thirst, constipation or confusion.
Pressure on the nerves in the spine (spinal cord compression) – Abnormal bone growth or
fractures can press on the nerves in the spine. This may cause back pain, muscle and limb weakness, tingling or numbness of the limbs, difficulty walking, or loss of bowel or bladder control.
Low levels of blood cells – Secondary bone cancer can affect the bone marrow, particularly if there is a large amount of spread to the bones. The bone marrow makes blood cells, so the cancer can lead to low levels of blood cells. Symptoms depend on the type of blood cells affected. You may feel tired and breathless, have an increased risk of infections, or bruise and bleed more easily.
What are the causes?
Secondary bone cancer is always caused by cancer cells that have spread to the bone from a primary cancer elsewhere in the body. It isn’t fully understood why some people develop secondary bone cancer and others don’t.
How is secondary bone cancer diagnosed?
Secondary bone cancer may be found at the same time as the primary cancer, or months or years after the primary cancer has been treated.
In some cases, secondary bone cancer is diagnosed before the primary cancer is found and, sometimes, the primary cancer can’t be found. When tests can’t find where the cancer started, this is known as cancer of unknown primary (CUP).
If your doctor is concerned the cancer has spread to the bones, you may have some tests, including a:
- blood test – usually a full blood count, a check of your calcium levels and possibly a specific blood test called an alkaline phosphatase (ALP) test
- bone x-ray – a scan to show bone damage, fractures or creation of new bone
- bone scan – a small amount of radioactive dye is injected into a vein; it collects in the bone and any abnormal changes are found by a special camera and computer
- CT or MRI scan – CT (computerised tomography) and MRI (magnetic resonance imaging) scans create detailed cross-sectional pictures to highlight any bone abnormality; they take between 30 and 60 minutes
- PET–CT scan – this is a PET (positron emission tomography) scan combined with a CT scan, which provides more detailed information than a CT on its own; you are injected with a small amount of radioactive glucose solution, which will highlight any cancerous areas on the scan
- bone biopsy – removal of some cells and tissue from the affected bone for examination under a microscope. The biopsy may be done in one of two ways. In a core needle biopsy, local anaesthetic numbs the area, then a thin needle is inserted to remove a sample of bone. In a surgical biopsy, a surgeon removes a small section of bone under general anaesthetic. The sample is sent to a pathologist who checks it for cancer cells.
Prognosis
Prognosis means the expected outcome of a disease. Factors affecting prognosis include whether the cancer has spread to other parts of your body, the type of primary cancer, how quickly it is growing and its response to treatment.
It is not possible for anyone to predict the exact course of the disease, but your doctor can provide you with general information on the expected outcomes of people in a similar situation to you and discuss treatment options. The expected outcome also depends on the site that the cancer started from (i.e. the prognosis of the primary cancer).
Secondary bone cancer can’t always be cured, but treatment can reduce symptoms and improve quality of life. In some cases, treatment can keep secondary bone cancer under control for many years.
Treatment for secondary bone cancer
The aim of treatment for secondary bone cancer is to control or shrink the cancer and relieve symptoms. This is called palliative treatment and may make you feel better.
Your treatment options will depend on:
- the type of primary cancer, if it is known
- the treatment you have already had
- how many bones are affected by cancer
- whether the cancer has spread to other parts of the body
- your symptoms and general health.
You may have treatment that affects the body as a whole (systemic) or focuses on a particular bone (local). Systemic treatments include hormone therapy, chemotherapy, targeted therapy, immunotherapy and bone-strengthening drugs. Local therapies include radiation therapy and surgery. Treatments can be given on their own or in combination.
Cancer treatments may cause a range of side effects, including fatigue, changes in appetite, hair loss and skin irritation. Talk to your doctor about managing any side effects you have. Ask your health professional whether you need to avoid any particular physical activity.
Radiation therapy
Also known as radiotherapy, radiation therapy uses targeted radiation to kill or damage cancer cells. The radiation is usually in the form of x-ray beams. Radiation therapy is often used to reduce pain in the bone. It is usually given from outside the body and is aimed at the particular bone causing pain.
The most common type of radiation therapy used for secondary bone cancer is external beam radiation therapy (EBRT). You will lie on a treatment table and a machine will deliver radiation to the affected area of the body. You may have one radiation therapy treatment, or several over a few days or weeks.
A type of EBRT called stereotactic body radiation therapy (SBRT) may also be used for secondary bone cancer. This is also known as stereotactic ablative body radiation therapy (SABR). You will lie on a treatment table and a machine will precisely deliver a few high doses of radiation to the bones. SBRT is offered in some specialised centres.
Depending on the cancer type, you may be injected with a small amount of radioactive liquid. This is known as radionuclide therapy (theranostic therapy). The liquid spreads throughout the body particularly targeting cancer cells. Your treatment team will let you know of any safety measures you need to follow.
Side effects – These relate to the type of cancer and the part of the body treated. They include
fatigue, skin problems, hair loss, low blood cell counts, appetite loss and nausea.
Chemotherapy
Chemotherapy uses drugs to kill or slow the growth of cancer cells, while causing the least possible damage to healthy cells.
Generally, chemotherapy is given through a vein (intravenously) over several hours, or as an injection between the skin and the muscle, or sometimes as a tablet (orally). Most people have several treatment cycles with rest periods in between. The number of sessions will vary depending on the drugs prescribed by your doctor and the type of primary cancer.
Side effects – These will depend on the chemotherapy drugs you receive. Common side effects include fatigue, nausea, diarrhoea, appetite loss, hair loss and increased risk of infections.
Targeted therapy
Targeted therapy uses drugs that attack certain features – genes or proteins – in the cancer cells to stop the cancer growing and spreading. The type of drugs you have will depend on the primary cancer.
Targeted therapy drugs can be given in different ways, including:
- as tablets that you swallow (orally)
- by injection under the skin (subcutaneously)
- by injection into a vein (intravenously).
Side effects – These will vary depending on the drugs used and how your body responds. Targeted therapy drugs often cause skin problems, such as dry, flaky skin and skin rashes. Other common side effects include fever, tiredness, joint aches, nausea, diarrhoea and headaches.
Immunotherapy
Immunotherapy is a type of drug treatment that uses the body’s own immune system to fight cancer. The most common immunotherapy used to treat secondary bone cancer is checkpoint inhibitor drugs.
Some cancers block the immune system by creating “checkpoints”. Checkpoint inhibitor drugs allow the immune system to recognise and attack cancer cells, bypassing these checkpoints.
Several checkpoint inhibitor drugs are approved to treat some types of cancer that have spread to the bone, such as melanoma, lung, bladder and kidney cancers. Clinical trials are testing checkpoint immunotherapy for other cancer types.
Side effects – These will depend on the type of treatment you receive and how your body responds. Common side effects of immunotherapy are fatigue, dry eyes, rashes and diarrhoea.
Hormone therapy
Hormone therapy, also called endocrine therapy, may be used to treat breast or prostate cancer that has spread to the bone. Synthetic hormones which have been produced in a laboratory are given as tablets or injections to slow or stop the effect of the body’s natural hormones. The aim is to reduce the amount of hormones reaching the cancer cells. This can help to slow down the growth and spread of the cancer.
Side effects – Common side effects include hot flushes, mood changes, weight changes and
sweating. Some types of hormone therapy can also weaken your bones, and affect your sex drive.
Surgery
Cancer can weaken bones and cause fractures. Surgery using metal rods or prostheses can be used to stabilise a fracture, or to strengthen bones which are at risk of fracturing. Surgery may also be used if the cancer is pressing on the spinal cord and causing weakness in the arms or legs.
Side effects – After surgery, some people develop an infection at the wound site. Your surgeon will discuss ways to prevent this happening.
Bone-strengthening drugs
Your doctor may prescribe medicines to help strengthen your bones, reduce bone pain and
control high calcium levels in the blood (a condition known as hypercalcaemia).
There are two options for bone-strengthening drug treatment:
- bisphosphonates – a group of drugs that can be given as an injection into a vein intravenously) or taken as a tablet (orally)
- denosumab – given as an injection under the skin (subcutaneously).
Side effects – These will vary depending on how the drugs are taken. Bisphosphonates taken
intravenously can cause muscle and joint pain, fatigue, nausea or flu-like symptoms, such as a sore throat, shivering and fever.
Bisphosphonates taken orally may make your throat sore, or cause indigestion or nausea. Occasionally, bisphosphonates can cause kidney damage. Your kidney function will be monitored with regular blood tests.
Side effects of denosumab are uncommon but can include nausea, fatigue, diarrhoea, constipation and bone, joint and muscle pain.
All bone-strengthening drugs can lower calcium levels, so your doctor may advise you to take calcium and vitamin D supplements.
A rare but severe side effect of bone-strengthening drugs is the breakdown of bone tissue in the jaw. Called osteonecrosis of the jaw or ONJ, this may happen after the removal of a tooth. See a dentist before starting to take bone strengthening drugs, and then every 6 months while taking these drugs. If you need to have dental work during treatment, let your dentist know that you are taking bone-strengthening drugs and ask your oncologist if you can have a break in treatment. See your doctor if you experience mouth ulcers, mouth pain or jaw problems while taking bone strengthening drugs.
Palliative treatment
Because secondary bone cancer is advanced cancer, your doctor is likely to discuss palliative treatment for symptoms caused by the cancer and to control the cancer for a period of time. Palliative treatment aims to manage symptoms without trying to cure the disease.
Palliative treatment is one aspect of palliative care, in which a team of health professionals aims to meet your physical, emotional, cultural, social and spiritual needs. The team also provides support to families and carers.
Download our booklet ‘Understanding Palliative Care’
Download our booklet ‘Living with Advanced Cancer’
Listen to our podcast series ‘The Thing About Advanced Cancer’
"I’ve been having palliative treatment for 5 years. I’m not trying to get rid of the disease, just keeping it under control. My quality of life is excellent.” KATE
Taking part in clinical trials
New treatments are constantly becoming available. Clinical trials test new treatments to see if they’re better than current methods. If you join a randomised trial for a new treatment, you will be chosen at random to receive either the best existing treatment or the modified new treatment. Talk with your doctor to see if there are any suitable trials for you.
Managing common symptoms
For many people with secondary bone cancer, managing symptoms may make you feel better.
Pain
Paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can be used to treat mild pain. Opioid-based medicines can help reduce moderate to severe pain. Steroids, like dexamethasone, are strong anti-inflammatory medicines and may be used for bone pain.
Fatigue
Many people experience extreme or constant tiredness known as fatigue. This may be because the cancer is affecting your bone marrow. You’ll have blood tests to monitor your blood cell count. If your red blood cell level is low (anaemia), you might have a blood transfusion. Getting enough rest, exercise and eating well can help with your energy levels.
Complementary therapies
These therapies are used alongside conventional medical treatments. Therapies such as massage,
relaxation and acupuncture can increase your sense of control, decrease stress and anxiety, manage pain and improve your mood. Let your doctor know about any therapies you are thinking about trying, as some may not be safe or evidence-based.
Living with secondary bone cancer
People diagnosed with secondary bone cancer can feel well and have long periods of time without symptoms. However, after finding out that you have advanced cancer, it’s natural to have a lot of different emotions. At times, you may feel overcome by fear, anxiety, sadness, depression or anger.
The uncertainty of living with secondary bone cancer can have a huge emotional impact. Your doctor, nurses, a social worker or counsellor can help you and your family find ways to cope with how you’re feeling. Get in touch with Cancer Council 13 11 20 for support.