The liver
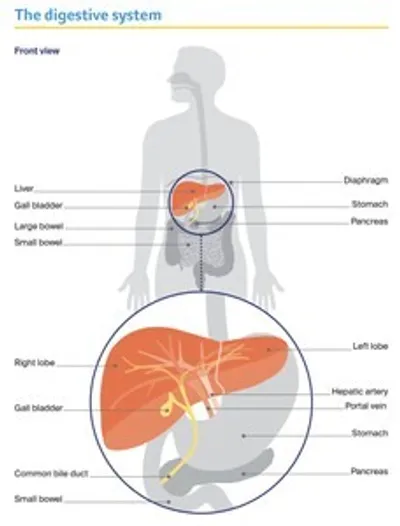
The liver is the largest organ inside the body, it is about the size of a football.
It is part of the digestive system, working with the gall bladder and pancreas to help break down food and turn it into energy.
The liver has many important jobs, including:
- storing sugars and fats, so they can be used for energy
- producing bile which helps dissolve fat so it can be easily digested
- making proteins to help blood clot and to balance fluid in the body
- breaking down harmful substances, such as drugs and alcohol.
The liver is found on the right side of the abdomen (belly) sitting just above the stomach and under the rib cage. The two main sections of the liver are the right and left lobes.
Blood flows into the liver from the hepatic artery and the portal vein. Blood in the hepatic artery comes from the heart and carries oxygen. Blood in the portal vein comes from the digestive organs and carries nutrients and substances (e.g. medicines) to the liver.
Unlike other internal organs, a healthy liver may be able to repair itself if it is injured or part of it is surgically removed during cancer treatment.
Key questions
Answers to some key questions about secondary liver cancer are below.
What is secondary liver cancer?
Cancer in the liver can be either a primary or secondary cancer. The two types of cancer are different. This information is only about secondary liver cancer.
Primary liver cancer – Cancer that starts in the liver is called primary liver cancer. The most common type is hepatocellular carcinoma (HCC).
For information about primary liver cancer, download our booklet ‘Understanding Liver Cancer’
Secondary liver cancer – Cancer cells from a primary cancer in another part of the body can spread from there to the liver via the bloodstream or lymph vessels. This is called secondary liver cancer, and it is much more common than primary liver cancer in Australia. Secondary cancers keep the name of the original cancer (for example, secondary liver cancer that started in the lung is called metastatic lung cancer). Because the cancer has spread, it is considered advanced cancer.
Which cancers spread to the liver?
Bowel cancer is the most common cancer that spreads to the liver. This is because the blood supply from the bowel is connected to the liver through a major vein called the portal vein. Other cancers that can spread to the liver include: breast, kidney, lung, melanoma, oesophageal, ovarian, pancreatic, prostate and stomach.
Sometimes, it’s not possible to find where the cancer started; this is called cancer of unknown primary (CUP).
If you have secondary liver cancer, you may find it useful to download our booklets about the primary cancer type or CUP.
What are the symptoms?
If the tumours are small, secondary liver cancer may have no symptoms. As the cancer grows or spreads, a range of symptoms may occur.
These may include:
- weakness and tiredness (fatigue)
- pain in the upper right side of the abdomen or right shoulder blade
- severe pain in the abdomen
- appetite loss and feeling sick (nausea)
- unexplained weight loss
- yellowing of the skin and eyes (jaundice)
- dark urine (wee) and pale faeces (poo)
- itchy skin
- a swollen abdomen (ascites)
- fever.
"Calling 13 11 20 after I was diagnosed helped me to take in the new information. Eventually, I joined a support group, which was also a great help.” LUISA
How is secondary liver cancer diagnosed?
Secondary liver cancer may be diagnosed at the same time as the primary cancer or up to several years after the primary cancer has been treated.
It may also be diagnosed before the primary cancer. Secondary liver cancer is found using several tests, including blood tests and imaging scans.
Blood tests
Blood tests alone cannot diagnose secondary liver cancer, but they can give doctors more information about the cancer.
Samples of your blood may be tested to check how well the liver is working (liver function tests) and to see if the liver is making proteins that help the blood clot.
Imaging scans
Various imaging scans may be needed when secondary liver cancer is suspected:
- You may first have an ultrasound scan, which helps to show if there is a tumour in the liver and how large it is.
- You will also have a CT (computerised tomography) scan and/or an MRI (magnetic resonance imaging) scan. These types of scans can provide more detail about the size of the cancer and the number of tumours.
- A PET (positron emission tomography) scan can be combined with a CT scan to provide even more detail about the cancer. This is called a PET–CT scan. Medicare does not always cover the cost of PET–CT scans for cancer diagnosis; if this test is recommended, check with your doctor if you will have to pay.
"At first, I found the MRI frightening, going into the cylinder and having to hold my breath. But now when I have this scan, I count to myself. This helps me feel more in control.” ROBYN
Biopsy
Occasionally, a tissue sample may be removed from the tumour to confirm a diagnosis of secondary liver cancer. This test is called a biopsy.
Tests to find the primary cancer
If test results show that you have secondary liver cancer, the next step is to work out where in the body the cancer started. This may be known if you have been treated for cancer in the past; otherwise, you will need further tests.
Sometimes, even after several tests, the primary cancer can’t be found. This is called cancer of unknown primary (CUP).
Depending on where your doctor thinks the primary cancer started, you may have:
- an examination of the bowel (colonoscopy), stomach (endoscopy) or breasts (mammogram)
- a urine test to show whether the kidneys and bladder are working properly
- a blood test to check for particular chemicals produced by cancer cells. These are known as tumour markers and they relate to the primary cancer – for example, bowel cancer sometimes produces a tumour marker called carcinoembryonic antigen (CEA).
Staging
Staging is the process of working out how far a cancer has spread through the body. Because the cancer has spread from another part of the body, secondary liver cancer is considered advanced cancer (also called stage 4 cancer).
The secondary cancer will be given a stage using the system for the primary cancer. For example, if it started in the bowel, it will often be staged using a system called TNM (tumour–nodes–metastasis). For more information about staging, download the Cancer Council booklet on the primary cancer.
Prognosis
Prognosis means the expected outcome of a disease. You may wish to discuss your prognosis with your doctor, but it is not possible for anyone to predict the exact course of the disease.
To work out your prognosis, your doctor will consider factors such as the type of primary cancer, the size and number of cancers in the liver, and how fast the cancer is growing. Your age, fitness and overall health will also affect your prognosis. Doctors often use numbers (statistics) when considering someone’s prognosis. While statistics give doctors a general idea about how a disease might progress, they won’t necessarily reflect your specific situation.
Although most cases of secondary liver cancer can’t be cured, surgery and other treatments can keep many cancers and symptoms under control for months or even many years.
Treatment for secondary liver cancer
The aim of treatment for secondary liver cancer depends on the type of primary cancer that has spread to the liver.
For some people, the aim may be to remove or destroy the cancer using surgery and chemotherapy. For others, the aim may be to shrink the cancer, manage symptoms and improve quality of life (called palliative treatment).
The types of treatment suitable for you will also depend on the size and number of tumours, and your age and general health.
The main treatment for secondary liver cancer is chemotherapy or a combination of surgery and chemotherapy.
Chemotherapy
Chemotherapy uses drugs to kill, shrink or slow the growth of cancer cells. The type of drugs you are given will depend on factors including your general health and where in the body the cancer started. If you have bowel cancer that has spread to the liver, for example, you will have chemotherapy designed to treat bowel cancer.
Depending on the treatment aim, chemotherapy may be given as a short course over a few months, or as a longer course over many months or years. The drugs can be given in different ways, such as being injected into a vein (intravenously) or swallowed as tablets.
Chemotherapy may be used at different times:
- before surgery, to shrink the secondary liver cancer and make it easier to remove (called neoadjuvant chemotherapy)
- after surgery, to get rid of any remaining cancer cells (called adjuvant chemotherapy)
- to slow down cancer growth and reduce symptoms such as pain (called palliative treatment).
Side effects – Chemotherapy drugs circulate throughout the body and can affect normal, healthy cells as well as cancer cells. People react to chemotherapy differently – some people have few side effects, while others have more. Side effects may include: nausea; loss of appetite; tiredness; hair loss; skin changes; tingling, numbness or pain in fingers and toes (peripheral neuropathy); and mouth sores. Most side effects last only while you are having treatment, and there are often ways to manage them.
During chemotherapy, you have a higher risk of bleeding or an infection. If you develop a temperature over 38°C, it’s important to contact your doctor or go to the emergency department as soon as possible.
Targeted therapy
This is a type of drug treatment that attacks specific features of cancer cells to stop the cancer growing and spreading. Targeted therapy drugs may be used in combination with other treatments.
Side effects – These vary depending on the drugs used, but may include high blood pressure, rashes, diarrhoea, and tender hands and feet. Talk to your doctor about ways to manage side effects.
Immunotherapy
Drug treatment that uses the body’s own immune system to fight cancer is called immunotherapy. Several immunotherapy drugs are available in Australia. The type of drug used for secondary liver cancer will depend on where the cancer started in your body.
Side effects – Immunotherapy drugs can cause a range of side effects; most are mild, but some are more severe. Most immunotherapy side effects can be managed and reversed if they are reported early.
Hormone therapy
Some cancers – such as prostate cancer and certain types of breast cancer – rely on hormones to survive and grow. If one of these types of cancer has spread to the liver, hormone therapy may be an option. This treatment can lower the levels of certain hormones in the body to help to control hormone-dependent cancers. Hormone therapy is usually used in combination with other cancer treatments.
Side effects – These may be different depending on the type of drug you have.
Radiation therapy
Also known as radiotherapy, radiation therapy uses targeted radiation to treat cancer. It can be delivered internally or externally. Specialised forms of radiation therapy – selective internal radiation therapy (SIRT) or stereotactic body radiation therapy (SBRT) – may be used to treat secondary liver cancer.
SIRT
This is the most common type of radiation therapy used for secondary liver cancer. Also called radioembolisation, SIRT may be offered when there are many small tumours in the liver that can’t be removed with surgery. It is usually needed only once.
SIRT precisely targets cancers in the liver with high doses of internal radiation. Tiny radioactive beads (made of glass or resin) are delivered through the blood vessels to the cancer. The radiation from these beads damages the cancer cells and their blood supply, while causing little damage to normal cells.
Side effects – You may have flu-like symptoms, nausea and pain, which can be managed with
medicines. Over the next week or so, you may need to take some safety precautions, such as not sharing a bed and avoiding close physical contact with children or pregnant women.
How SIRT is done
Selective internal radiation therapy (SIRT) combines embolisation (which blocks blood supply to the tumour) with internal radiation therapy.
SBRT
An increasing number of cancer centres now offer SBRT, which is also called stereotactic ablative body radiation therapy (SABR). SBRT is a type of external beam radiation therapy. It may be offered to some people with small secondary tumours in the liver.
You will be asked to lie very still on a treatment table. A machine will precisely target beams of radiation from many different angles onto the tumour. The highly targeted radiation means surrounding healthy tissue is protected. SBRT requires fewer treatment sessions than conventional external beam radiation therapy. People may need only 3–8 sessions over one or two weeks.
Side effects – These may include fatigue, nausea, and soreness in the treatment area.
Transarterial chemoembolisation (TACE)
Transarterial chemoembolisation (TACE) is sometimes used in people with secondary liver
cancer who can’t have surgery or ablation. In TACE, chemotherapy drugs are delivered directly to the tumour through the hepatic artery. The chemotherapy will either be mixed with an oily substance or loaded onto tiny plastic beads. The blood vessel feeding the tumour may also be blocked (embolisation).
Side effects – It is common to have a fever the day after the procedure, but this usually passes quickly. You may have nausea and vomiting, or feel some pain, which can be controlled with medicines. Some people may feel tired or have flu-like symptoms for up to a week after the procedure.
Tumour ablation
Applying heat or alcohol (ethanol) directly to the tumour without removing it is called tumour ablation. Thermal ablation, which uses microwaves or radiofrequency to generate heat, is the most common method used. In secondary liver cancer, tumour ablation may be used in combination with chemotherapy or surgery.
Surgery
A small number of people with secondary liver cancer may be able to have surgery to remove the cancer (also known as liver resection or partial hepatectomy). A liver resection is only an option for people with some types of secondary cancer and when there will be enough healthy liver for it to regrow. Surgery is also only possible when the cancer hasn’t spread to other parts of the body where it can’t be removed, such as the bones.
A liver resection is a major operation. You will have a general anaesthetic and the surgeon will remove the cancer as well as some healthy tissue around it. The operation may be done as open surgery (with one large cut in the abdomen) or as keyhole or laparoscopic surgery (with several smaller cuts).
When a large amount of the liver needs to be removed, you may have a procedure called portal vein embolisation (PVE) 4–8 weeks before the surgery. This procedure redirects the blood supply to the healthy part of the liver, helping it to grow.
People with tumours in both lobes of the liver sometimes need two separate operations with a waiting period between each operation.
After the surgery – You will spend 5–10 days in hospital. You will be monitored for signs of infection or bleeding. Some people develop jaundice (yellowing of the skin and whites of the eyes), but this is usually temporary and improves as the liver grows back. The liver will usually regrow to its normal size within a few months.
Palliative treatment
Secondary liver cancer is advanced cancer so your doctor is likely to discuss palliative treatment. This helps to improve people’s quality of life by managing the symptoms and spread of cancer without trying to cure the disease. Many people think that palliative treatment is for people at the end of their life, but it may help at any stage of secondary liver cancer. It is about living for as long as possible in the most satisfying way you can.
Palliative treatment may include chemotherapy, targeted therapy, immunotherapy, other medicines, radiation therapy or stenting. Palliative treatment is one aspect of palliative care, in which a team of health professionals aims to meet your physical, emotional, cultural, social and spiritual needs. The team also provides support to families and carers.
Managing symptoms
Secondary liver cancer can cause various symptoms, but there are ways to manage them.
As this is an advanced cancer, the palliative care team may be involved in managing symptoms.
Jaundice
Bilirubin is a yellow pigment formed when red blood cells in the body break down. In secondary liver cancer, bilirubin sometimes builds up in the blood. This can be because the cancer has blocked a bile duct or affected how the liver is working.
The build-up of bilirubin in the blood is known as jaundice. It can cause yellowing of the skin and whites of the eyes. People with jaundice may feel very tired and lose their appetite.
Jaundice can also cause pale faeces, dark urine and itchy skin, which is often worse at night. Try to avoid alcohol, spicy food, hot baths and direct sunlight, which can make the itching worse. Keeping your skin moisturised can provide some relief, or your doctor can prescribe medicine that may help.
Jaundice can sometimes be relieved by inserting a small tube made of plastic or metal (a stent) into the bile duct. Symptoms of jaundice usually go away 2–3 weeks after the stent is placed into the bile duct. However, stenting is not always recommended or possible in advanced cancer.
Poor appetite and weight loss
Because the liver plays a key role in the digestive system, secondary liver cancer can affect your appetite and you may lose weight.
Chemotherapy, radiation therapy and other cancer treatments can also have an impact on appetite and weight, especially if you have side effects such as nausea and vomiting, mouth ulcers, and taste and smell changes.
How to stay well nourished
During and after treatment, it’s important to eat and drink enough to keep your energy levels up. Maintaining your weight can help your recovery.
Eat foods you enjoy – Eat foods that you like, but also try different foods; your taste and tolerance to some foods may change. Chew foods well and slowly. Keep a selection of snacks handy (e.g. in your bag or in the car).
Drink liquids – Prevent dehydration by drinking liquids between meals (e.g. 30-60 minutes before or after meals). Avoid filling up on liquids at mealtimes – unless it’s a hearty soup.
Ask for advice and help – Talk to a dietitian about how you can add more energy and protein to your meals. Ask your friends and family to cook for you and offer you food throughout the day. Try having small, frequent meals or snacks rather than three large meals each day.
Download our booklet ‘Nutrition for People Living with Cancer’
Pain
In some people, secondary liver cancer can cause pain, particularly in the upper right area of the abdomen (belly). Your doctor may prescribe pain medicine, but check before taking any over-the-counter medicines because some are not suitable for people with liver cancer.
Radiation therapy, chemotherapy or surgery may also provide relief by reducing the size of a liver tumour that is causing pain. Some people may have an injection of local anaesthetic to numb the nerve sending the pain signals (nerve block).
Fatigue
Many people with secondary liver cancer experience fatigue. This is different to feeling tired as it doesn’t always go away with rest or sleep. Fatigue may be a side effect of treatment or caused by the cancer.
Fluid build-up
Ascites is when fluid builds up in the abdomen (belly). It can be caused by the cancer producing extra fluid or blocking lymph vessels from draining fluid. This fluid build-up causes swelling in the abdomen, which can be uncomfortable and may make you feel breathless. Draining the fluid with a procedure called paracentesis or ascitic tap can help. Diuretics (water tablets) may also be prescribed to reduce the build-up of fluid.
Confusion
Secondary liver cancer may cause toxic substances to build up in the blood, which can affect brain function. Called hepatic encephalopathy, this can lead to confusion or disorientation and, in severe cases, coma. Hepatic encephalopathy can be controlled with medicines.
Living with secondary liver cancer
Some people diagnosed with secondary liver cancer can feel well and have periods of time without symptoms.
But the uncertainty of living with cancer that cannot be cured can have a huge emotional impact. At times, you may feel overcome by fear, anxiety, sadness or anger.
Your doctor, nurses, a social worker or counsellor can help you and your family find ways to cope with how you are feeling.